Spina Bifida
Overview
The entire human nervous system develops from a plate of specialized cells that form along the back of the embryo. The edges of this elongated plate curl toward each other and join in as many as 4 places to form a tube. It then proceeds caudally (tailward) to where the end of the spinal cord forms and cephalad (toward the head) where further specialization leads to brain development. Spina bifida results from problems during this complex process in which genetic and environmental factors are involved. [Kaufman: 2004] [Finnell: 2003] Defects can be classified as open (spina bifida) or closed (spina bifida occulta, diastematomyelia).
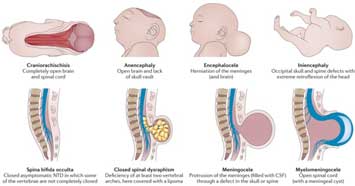
- Myelomeningocele: This is the most common symptomatic and severe form of spina bifida. The spinal cord and the meninges protrude through the posterior openings in the vertebrae.
- Meningocele: The meninges protrude through the posterior openings in the vertebrae, but the spinal cord is not involved, although spinal nerves may be.
- Spina bifida occulta: There is an opening or defect in 1 or more vertebrae with no pathology in the spinal cord. This is generally asymptomatic and will not be discussed further.
- Closed neural tube defects: These are a rare, diverse group of defects where the spinal cord is malformed, but the vertebral column is intact. These include lumbosacral lipomas and diastematomyelia. These defects may range from mild to very severe. Infants with these defects may be asymptomatic at birth and then develop symptoms over time. Midline sacral skin tags, hairy patches, hemangiomata, and other cutaneous markers may signal the presence of a closed neural tube defect and should be looked for in all newborns. [Brand: 2007]
While 90% of children born with spina bifida have no family history of spina bifida, risk factors include:
- Maternal folic acid deficiency - see Folic Acid Supplementation & Neural Tube Defects and [Kancherla: 2018] for more details
- A previous NTD-affected pregnancy, whether it be spina bifida, anencephaly, etc.
- Maternal insulin-dependent diabetes
- Use of certain anti-seizure/mood-stabilizing medications (valproic acid and carbamazepine) during pregnancy
- Medically diagnosed obesity in the mother
- Exposure to high temperature in early pregnancy (prolonged fever or hot tub use)
- Maternal race/ethnicity (more common among white women than black women and more common among Hispanic women than non-Hispanic women) [National: 2019]
- Lower maternal socio-economic status
Other Names & Coding
Q05.x, Spina bifida
The “x” above indicates the need for additional specificity (defect position and with/without hydrocephalus); for details, see ICD-10 for Spina Bifida (icd10data.com).
Prevalence
Genetics
Prognosis
Practice Guidelines
Spina Bifida Association.
Guidelines for the management of spina bifida.
2018; https://www.spinabifidaassociation.org/guidelines/
This 4th edition is evidence based, where evidence exists, and otherwise based on expert opinion. It includes 25 topics for
care of the individual with spina bifida from birth through adulthood. Recent additions include an emphasis on coordination
of care, multidisciplinary care, and culturally sensitive care.
Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW Jr, García FA, Kemper AR, Krist AH, Kurth AE, Landefeld CS,
Mangione CM, Phillips WR, Phipps MG, Pignone MP, Silverstein M, Tseng CW.
Folic acid supplementation for the prevention of neural tube defects.
JAMA/ US Preventive Services Task Force Recommendation Statement (USPSTF).
2017;317(2):183-189.
PubMed abstract
Roles of the Medical Home
Clinical Assessment
Overview
One randomized control trial (MOMs Trial) showed that prenatal surgery led to a decreased need for shunting, improved motor and mental development scores at 30 months post-gestational age, improved ambulation scores, and decreased hindbrain herniation; however, it was associated with significant risks for both the mom and the baby, including preterm labor and uterine dehiscence at delivery. [Adzick: 2011] Although this section will focus on the initial evaluation and management of children with spina bifida, infants born after fetal surgery will still need to be followed for many of the same problems, such as lower urinary tract dysfunction, which does not improve with fetal surgery, hydrocephalus, and other issues. [Lee: 2012]
Most infants with spina bifida will undergo surgery soon after birth to repair the defect and accompanying hydrocephalus if present. During the initial hospitalization (birth), protocol for care includes an echocardiogram, head ultrasound, renal ultrasound, and initiation of a latex-free environment.
Pearls & Alerts for Assessment
Undescended testiclesAs many as 1:4 males with NTDs will have undescended testicles. [Meyer: 1984]
Screening
For the Condition
Diagnostic Criteria
Comorbid & Secondary Conditions
- Abnormal spinal cord development results in some degree of paralysis or muscle weakness and sensory loss below the level of the defect. The neurologic lesions are complicated and unique for each child. The paralysis is most likely to be a flaccid paralysis, although tethered cord and other accompanying defects may lead to lower extremity spasticity. Mobility is usually affected.
- Hydrocephalus and abnormal brain development are common. Most children with the myelomeningocele type of spina bifida also have hydrocephalus (70-90%) and may need a shunt or other procedures to relieve the fluid pressure in the brain. Children with myelomeningocele may also have abnormal brain development (Chiari II, thinning of the corpus callosum with decreased neuron content in the posterior region of the brain, heterotopic grey matter, and other).
- Bowel and bladder dysfunction are almost universal, even in low sacral lesions, and significantly affect morbidity, mortality, and quality of life.
- Neurogenic bladder occurs because the bladders of children with spina bifida are paralyzed (neurogenic), and reflux of urine up the ureters and into the kidneys (vesicoureteral reflux) can occur. This can lead to kidney failure, particularly in the setting of frequent urinary tract infections.
- Lack of skin sensation, including feelings of pain, pressure, friction, heat, and cold, which may contribute to skin problems.
- Constipation and other gastrointestinal problems
- Latex allergy
- Skin breakdown
- Orthopedic problems
- Learning and mood problems
History & Examination
Current & Past Medical History
- Level of the spinal lesion, surgical repair and results, movement and sensation below lesion
- Bladder and bowel function
- Urinary tract screening (usually ultrasound and voiding cystourethrogram) results
- Brain involvement (Chiari II malformation, treated or untreated hydrocephalus)
- Presence or absence of seizures
- Family adjustment and acceptance
- Enrollment in an Early Intervention program
Pregnancy/Perinatal History
Developmental & Educational Progress
Maturationalprogress
Social & Family Functioning
Physical Exam
General
Vital Signs
Growth Parameters
Length or height | weight | BMI | OFC: Follow weight and length for
adequate growth. For a child who is unable to stand, consider following
length (as opposed to height) or a substitute measure, such as length from
foot to knee or arm span, understanding that translation to a height growth
chart may be initially misleading.
Follow OFC for
increasing percentiles that may signal hydrocephalus. Head circumference
should be followed until there is no further growth, particularly in
children with a history of hydrocephalus and shunting.
Skin
Abdomen
Feel for kidneys (hydronephrosis) and masses that suggest constipation. Check anal sphincter tone initially and as clinically indicated afterwards. In male infants, observe urinary stream if possible.
Extremities/Musculoskeletal
Look for spinal deformities, such as kyphosis and scoliosis. Check hips for clicks and dislocation. Clubfeet may be present.
Neurologic Exam
In infants, check for gag and suck reflexes. Test reflexes and confirm level of lesion – baseline is important if there is a subsequent question of deterioration (e.g., due to tethered cord, increased intracranial pressure). Evaluate muscle bulk and tone, presence of spontaneous and responsive movement, sensation in extremities and trunk; usually, the level of sensory dysfunction is slightly higher than that of motor dysfunction.
Testing
Sensory Testing
Laboratory Testing
Imaging
Other Testing
Specialty Collaborations & Other Services
Spina Bifida Clinics (see NW providers [1])
Pediatric Urology (see NW providers [0])
Pediatric Neurosurgery (see NW providers [1])
Pediatric Orthopedics (see NW providers [4])
Pediatric Physical Medicine & Rehabilitation (see NW providers [3])
Developmental - Behavioral Pediatrics (see NW providers [1])
Pediatric Neurology (see NW providers [0])
Food & Nutrition > … (see NW providers [3])
Colorectal Care Clinics (see NW providers [0])
Pediatric Gastroenterology (see NW providers [0])
Pediatric Gastroenterology (see NW providers [0])
Neuropsychiatry/Neuropsychology (see NW providers [0])
Educational Advocacy (see NW providers [5])
Treatment & Management
Overview
Pearls & Alerts for Treatment & Management
Third ventriculostomy and choroid plexus cauterizationThird ventriculostomy and concomitant choroid plexus cauterization is a technique for control of hydrocephalus for infants/children with hydrocephalus after fetal or postnatal surgery. When compared to shunt surgeries, it may improve hydrocephalus outcomes while avoiding the risks of shunts. This technique may be particularly helpful in developing countries. [Sufianov: 2010] [Duru: 2018]
Fractures due to osteoporosisFractures due to osteoporosis are common in non-ambulatory children, especially if additional risk factors are present (e.g., the child is taking valproic acid or has a proton pump inhibitor). Children with spina bifida should be maintained on a diet with adequate calcium and vitamin D; weight-bearing with braces or a standing apparatus should be encouraged. Although there are no guidelines for treatment in individuals with spina bifida, bisphosphonates, provided in collaboration with pediatric endocrinology, should be considered if there have been multiple fractures. [Marreiros: 2012]
How should common problems be managed differently in children with Spina Bifida?
Common Complaints
Systems
Neurology
Many children (60-80%) with spina bifida will require treatment and ongoing management for hydrocephalus, including those who have had fetal or post-natal surgery. Early recognition is key to minimizing its impact and sequelae.
Initial signs of hydrocephalus in infants, which may be subtle, include sleepiness, irritability, vomiting, sunsetting eyes, a bulging or full fontanelle, splayed sutures, and seizures, as well as a large and/or rapidly increasing head circumference. In children whose sutures have fused, signs/symptoms include nausea, headache, sunsetting eyes, balance problems, irritability, seizures, and visual disturbances, such as diplopia and blurred vision. Hydrocephalus that is slowly developing may be difficult to recognize because of more subtle and slowly evolving changes, such as a plateau or regression in developmental milestones, new learning problems, memory loss, difficulty concentrating, feeding difficulties, or personality changes.
Symptomatic hydrocephalus will require either shunt placement or, in some cases, a third ventriculostomy with choroid plexus cauterization (ETV+CPC). [Sufianov: 2010] The decision on the timing of shunt placement or ETV+CPC must balance the risks of surgery and related complications with potential brain damage from hydrocephalus. Nobody knows if a child with small ventricles and a shunt will do better than a child with stable, large ventricles. Although a pre-surgery MRI is helpful, the decision on which operation to do will ultimately be made during surgery.
Shunts
The most typical approach is a ventriculo-peritoneal (VP) shunt, the risks of which include:
- Shunt malfunction, resulting from obstruction by biologic debris or mechanical failure
- Obstruction or underdrainage, resulting in continued, increased intracranial pressure and symptoms
- Overdrainage, which may lead to subdural hematomas or slit ventricle syndrome and cause intermittent symptoms
- Abdominal complications, such as intestinal obstruction
- Infections, which are more common in the first few months after shunt placement and often due to Staphylococcus species
ETV+CPC
A third ventriculostomy involves a small hole made in the floor of the third ventricle to allow the CSF to escape the ventricular system to the space surrounding the brain, thus bypassing the obstruction. The choroid plexus, within the ventricles, makes 80% of the CSF. Coagulation of the choroid plexus is done through a single burr hole in the skull through which the neurosurgeon can coagulate the choroid plexus on both sides of the brain. If an ETV+CPC is successful, some of the problems of shunts, such as obstruction and failure, are eliminated.
Risks of an ETV+CPC include:
- Procedure abandonment due to hemorrhage or dangerous anatomy
- Meningitis
- Seizures
- CSF leak
- Major arterial injury (rare)
- Failure and subsequent need for a shunt
Although shunting in the first few weeks of life may improve neurodevelopmental outcome [Sgouros: 2006], many other factors, such as the degree of brain malformation, affect ultimate intellectual and functional outcomes. It is possible that ETV-CPC will improve outcomes over those achieved with shunts; data are not yet available comparing these 2 treatments, although it appears that children with ETV-CPC will need fewer additional procedures than those with a VP shunt.
Chiari II malformation
Chiari II malformation involves displacement of the cerebellar tonsils and inferior vermis, and possibly the fourth ventricle, choroid plexus, and medulla, into the spinal canal. It is present in virtually all patients with the myelomeningocele type of spina bifida but requires treatment in only a minority.
Symptoms of Chiari II malformation may be difficult to distinguish from those of shunt malfunction or increasing hydrocephalus in unshunted individuals. Infants with Chiari II may present with difficulty breathing, increased high-pitched crying, apneic episodes, aspiration, and arching (similar to that seen in infants with reflux). If syringomyelia is present, individuals may present with spasticity and/or progressive weakness. Older children present less dramatically but may have headache, swallowing difficulties, and passing out episodes. If Chiari II is suspected, imaging or a referral to Neurosurgery for management is recommended.
Tethered cord
Some children with spina bifida will have a tethered cord where the spinal cord, which is normally able to move and grow with the child, is fixed to the dura, scar tissue from a previous operation, or a bony spicule. The spinal cord becomes increasingly stretched as the spine grows in length, leading to damage to nerves that control the bowel, bladder, and legs.
The cord is also sometimes tethered in children with spina bifida occulta and other closed neural tube defects, such as diastematomyelia. Certain skin findings over the lower part of the back, including fat deposition, a hairy or discolored patch of skin, skin tags, and dimples may signal the presence of a tethered cord.
Symptoms may include back and associated leg pain, worsening ambulation and/or stamina, bowel or bladder problems, and/or orthopedic problems including back or leg pain, scoliosis, new or changing joint contractures, and weakness and loss of sensation in the legs. Increased tightness or spasticity in the legs leading to decreased range of motion may also be noted.
Symptoms of tethered cord might be subtle, especially in a child who use a wheelchair where gait problems will not be noted. Younger children may present with a decrease in activity, failure of toilet training, or wet diapers between catheterizations in those with neurogenic bladder.
Tethered spinal cord syndrome is principally diagnosed clinically; an MRI of the spine may demonstrate worsening tethered appearance or a syrinx (fluid-filled cavity within the spinal cord). In some cases, surgery is needed to release the spinal cord; however, there is controversy regarding the threshold of signs and symptoms at which surgery is necessary. Surgery may be helpful in preventing further deterioration and irreversible damage; however, only about 1/2 of the patients return to their pre-tethering baseline state with surgery. Tethered cord can recur in about 1/4 of children who have had release surgery. An international partnership has been established to address questions regarding diagnosis and optimal times to repair tethered cords for best outcome. [Mulholland: 2011]
Epilepsy
Seizures and epilepsy in children with myelomeningocele occur in 10-25% of affected children. [Talwar: 1995] [Noetzel: 1991] [Yoshida: 2006] In general, most studies have found epilepsy to be more prevalent in patients with hydrocephalus. [Noetzel: 1991] The presence of shunts and shunt revisions are not correlated with epilepsy. [Klepper: 1998]
Children with myelomeningocele and epilepsy tend to have other brain abnormalities, such as polymicrogyria or agenesis of the corpus callosum, and they may be more likely to have intellectual disability than those without epilepsy and may be more likely to have intellectual disability than those without epilepsy. [Talwar: 1995] [Yoshida: 2006] [Noetzel: 1991]
Seizures in children with spina bifida are treated similarly to seizures in the general population. See Seizures/Epilepsy for management. Unless the child has confounding factors of intellectual disability and/or hydrocephalus, the prognosis is generally good for seizure control. [Noetzel: 1991]
Specialty Collaborations & Other Services
Pediatric Neurosurgery (see NW providers [1])
Pediatric Neurology (see NW providers [0])
Genito-Urinary
Clean intermittent catheterization (CIC)
CIC and other improvements in care of the urinary system have greatly increased life expectancy in children with spina bifida. [Pruitt: 2012] At some point, 80% of individuals will require CIC for bladder management to either improve drainage and reduce bladder pressures or reflux, decrease urinary stasis and risk of urinary tract infections, or help achieve continence. Most babies with spina bifida are sent home from the hospital on a regimen of clean intermittent catheterization, taught to families before discharge.
Current management, as recommended in a CDC-sponsored, consensus-based protocol, is to begin all babies on a cathing program, but stop intermittent cathing if bladder volumes are less than 30 ml. on the majority of caths for 3 consecutive days. If bladder volumes do not meet these criteria, then babies are discharged on CIC every 4 hours while awake.
As part of the protocol, all babies with spina bifida are evaluated with videourodynamics (VUDS) and a renal/bladder ultrasound by 3 months of age to stratify their risk (normal/safe, low, intermediate, or hostile). Only those with hostile or high-risk bladder findings will be started on CIC, anticholinergics, and prophylactic antibiotics. These findings include any of the following:
- End-filling pressure or leak-point pressure greater than 40cmH2O
- Significant neurogenic detrusor over-activity and dyssynergia
- Grade V reflux by video urodynamics
- Grade 4 hydronephrosis on ultrasound
For older children and adults, urinary continence becomes a focus to help with self-esteem and socialization; adults identify continence as a major concern related to sexual intimacy. [Edwards: 2004] As continence is desired, urodynamics again have a role in management to ensure that typical toileting occurs at safe pressures with or without medications; the majority of patients will also require intermittent catheterization.
Medications
If required, anticholinergics are initiated with oxybutynin 0.2mg/kg TID. Antibiotic prophylaxis is initiated as a single daily dose with amoxicillin 15mg/kg until 2 months of age. After 2 months of age, prophylaxis is changed to sulfa suspension 2ml/kg or nitrofurantoin suspension 1-2mg/kg.
Encourage adherence to catheterization, if recommended, and have a low threshold for testing for urinary tract infections. Signs and symptoms of urinary tract infections include chills/fever, nausea/vomiting, pain in the lower back or abdomen, discomfort with catheterizations, blood in urine, general signs of illness, or foul-smelling, cloudy, or dark urine. It is sometimes difficult to determine if an individual who performs clean intermittent catheterization has an infection or benign bacteuria; current recommendations are to treat only symptomatic, culture-positive infections. In a study performed in 2005, no consensus was found among Spina Bifida Clinics in the United States regarding the management of bacteriuria. [Elliott: 2005]
Surgical management
Surgical diversion may also be required to help prevent kidney damage and/or achieve urinary continence if more conservative measures fail.
- Urinary diversion in the form of a vesicostomy can be performed, where an opening is created between the bladder and the abdomen to allow leaking into a diaper to keep urine volumes and bladder pressures low. This procedure is used when the bladder is not emptying sufficiently due to high outlet resistance, resulting in vesico-ureteral reflux. Usually this opening is closed when the child is older and ready for more definitive bladder surgery.
- Continence procedures may include a catheterizable urinary channel created from the abdomen into the bladder. These are called a Mitrofanoff when made of the appendix, Monti if made of bowel, continent vesicostomy if made of bladder tissue. A tube is left in the opening after surgery to allow the wound to heal and then removed. The opening can then be catheterized using clean intermittent catheterization.
- Antireflux procedures may include either injections
of a bulking agent or ureteral reimplantation.
- Cystoscopic injection of a bulking agent (typically Deflux) into the bladder wall under and above the ureter can enhance valve mechanism and prevent reflux.
- Re-implantation of ureters is done through an abdominal incision, creating a longer, steeper tunnel within the bladder wall to prevent reflux. This is performed when clean intermittent catheterization and medications have not been effective at preventing febrile urinary tract infections or renal scarring.
- Cystoscopic injections of Botox to the bladder can be an effective temporizing measure for some hostile bladders.
- Bladder augmentation to increase bladder capacity may be required to manage a hostile bladder or help achieve continence. This procedure is often done with a catheterizable channel.
- Outlet procedures are performed when the sphincter is not strong enough to prevent leaking between catheterizations. This may involve cystoscopic injection of a bulking agent, bladder neck reconstruction with an abdominal fascial sling, or, in some cases, an artificial urethral sphincter. These procedures are often performed with a catheterizable stoma to maintain integrity of the reconstruction, as well as bladder augmentation to maintain safe storage pressures. With outlet procedures, there is improved continence but a high rate of revision.
Specialty Collaborations & Other Services
Pediatric Urology (see NW providers [0])
Gastro-Intestinal & Bowel Function
Although non-surgical options should be tried first, occasionally, a colostomy or an ACE procedure (antegrade continent enema) may be needed for severe problems with constipation. The latter operation creates an opening between the skin of the abdomen and the proximal large intestine – an appendicostomy. This allows patients or their caregivers to administer fluids by inserting a catheter and flushing stool down the intestine. [Webb: 1998]
Specialty Collaborations & Other Services
Spina Bifida Clinics (see NW providers [1])
Colorectal Care Clinics (see NW providers [0])
Pediatric Gastroenterology (see NW providers [0])
Nutrition/Growth/Bone
Children who have decreased mobility and are on certain medications are more susceptible to fractures. Calcium and Vitamin D intake should be monitored and supplemented as needed. Also, see Osteoporosis and Pathologic Fractures.
Specialty Collaborations & Other Services
Dieticians and Nutritionists (see NW providers [1])
Learning/Education/Schools
Intelligence, learning problems, self-care, and independence
Although the IQ of children with spina bifida averages less than the general population, lower scores are generally found in children with hydrocephalus and higher spinal cord lesions, as well as in those with a history of central nervous system infection. [Lollar: 1995] Children with myelomeningocele have difficulty with perceptual motor skills and this tends to bring the full scale IQ down, whereas verbal intelligence scores are closer to the normal range. Children with myelomeningocele will generally do better in reading and writing than in math.
Even with normal intelligence, children with spina bifida often have difficulties with perceptual motor skills, organization, memory, sequencing, problem-solving, and attention, and they score poorly on measures of self-care, such as the WeeFim (Functional Independence Measure for Children) and the PEDI (Pediatric Evaluation of Disability Inventory).
Neuropsychological testing
Children with spina bifida and difficulty in school should be assessed with a full neuropsychological profile if the child is not age-appropriate or exhibits poor school performance. A neuropsychological profile helps to identify strengths and weaknesses and guide teaching methods for maximizing the child's potential. Funding for a full profile can be hard to obtain; school districts and/or the patient's insurance may be helpful, but they often require letters from the medical home clinician requesting the testing. Reassessments may be necessary as the child transitions to junior high and high school. The medical home can further help with school issues by tracking progress, school accommodations for learning problems, accessibility to all areas of the school, and a school health plan. An Individualized Education Plan (IEP) and a "504 Plan" should be developed and implemented for every child with spina bifida; School Accommodations: IEPs & 504s can help with this.
Skin & Appearance
Individuals, especially adolescents and adults with myelomeningocele, often develop decubitus ulcers in major weight-bearing areas, such as the buttocks and feet. Decubitus ulcers may eventually require prolonged hospital stays and, if not properly cared for, may be life-threatening. Early changes leading to decubiti may include blanching erythema (that does not resolve quickly after the pressure has been removed), warmth, and a feeling of hardness to the skin. As progression occurs, the erythema no longer blanches, or a white area is noted. The underlying bone, muscle, and/or joint capsule may be affected, and often the seriousness of the ulcer cannot be appreciated from observing the skin alone.
The family should participate in ongoing education about prevention and learn about pressure releases while in a wheelchair (10-second lifts every 15 minutes); frequent changes in positioning (for example, from a wheelchair to a mat every hour or 2 while at school); and, position changes every 2 hours while lying in bed. The first step in treating a pressure sore is to remove the pressure causing it. Consider new wheelchair cushions, a change in orthotics, or, if it is exacerbated by a contracture, antispasticity agents and a referral to surgery to release the contracture. If the decubitus is mild, thorough cleansing and possibly an occlusive dressing to keep the area moist may be sufficient. More advanced sores may require other types of dressings (wet to dry dressings, Carrington gel), intravenous antibiotics, whirlpool treatments, and surgical debridement/skin grafting.
Latex allergy
A large percentage of children with spina bifida have latex sensitivity and allergy with symptoms ranging from itchy and watery eyes to hives and fatal anaphylactic reactions. All children with spina bifida and their families should be taught to avoid latex in their environment. Newborns with spina bifida are usually put on latex precautions at birth. Although there are correlations with the latex exposure history, number of previous surgeries, and presence of other allergies, the intricacies of this allergy are not well understood. Because latex exposure to mucous membranes seems to correlate with increasing difficulty with latex allergy, sexually active adolescents and adults with spina bifida should use latex-free condoms. Specific recommendations for avoidance and lists of products that contain latex can be found at Latex Information (Spina Bifida Association).
Musculoskeletal
Although individual spina bifida lesions are unique and often complicated, generalizations on future mobility can be made based on the level of the lesion.
- Children with sacral lesions will often be able to walk, with or without braces, though usually later than typical children walk.
- Children with lower to mid-lumbar lesions will require more support to walk, including crutches, walkers, and/or bracing. These children will often become wheelchair-dependent as they move into adolescence.
- Children with high lumbar or thoracic lesions will usually be wheelchair dependent. Children with higher lesions that involve the upper extremities may need motorized wheelchairs for mobility. Note that power chairs can be used at developmental levels as young as 2 or 3 years.
Individuals with spina bifida commonly have musculoskeletal problems. These individuals should be followed by orthopedics at least yearly. Orthopedic issues include:
- Scoliosis
- Kyphosis
- Hip dislocations
- Foot and knee deformities
Kyphosis, curvature of the spine in an anterior-posterior plane, can cause progressive problems with seating, positioning, and pressure sores on the skin overlying the convex side. It can also lead to compression of abdominal contents and secondary interference with the function of the diaphragm and breathing. Kyphosis can be very difficult to manage, often requiring major spinal surgery to correct the deformity. Kyphosis accounts for about 10 % of spine defects, so it is less common than scoliosis in children with spina bifida. It is more common when the myelomeningocele lesion is above T12. [Foster: 2007]
Hip dislocations are common in children with spina bifida, increasing in incidence with higher lesions. Muscle release surgeries may decrease the forces dislocating the hips. Abnormal range of movement or pain with movement may signal the need for X-rays of the pelvis and a referral to orthopedics if a dislocation is present. Bone surgery can correct the deformities resulting from the muscle imbalance, improve the range of motion of the hips and knees, and facilitate bracing and standing. The decision to surgically treat hip dislocation is often based on the child's potential to walk, which is correlated with a lower lesion level (L3 level), the presence/absence of significant pain, and whether the dislocation is unilateral or bilateral.
Foot deformities are common in young children with spina bifida and may require bracing if the deformity is flexible. If the deformity is rigid, corrective surgery can relax the foot so that bracing can be effective.
Specialty Collaborations & Other Services
Pediatric Orthopedics (see NW providers [4])
Hospitals (see NW providers [3])
Maturation/Sexual/Reproductive
For unknown reasons, children with spina bifida and hydrocephalus often exhibit precocious puberty. This occurs more frequently in girls (possibly as high as 50% of girls with spina bifida). [Proos: 1996] Signs of early changes include breast development in girls and testicular enlargement and the development of pubic hair and acne in boys. Precocious puberty causes an early growth spurt, leading to decreased adult height and mood changes commonly seen in adolescence, such as moodiness, increased aggressiveness in boys, and sexual readiness, before the family and schools anticipate these changes. [Liptak: 2003] Testing may include bone age, ultrasound examination for uterine size, blood testing for elevated levels of sex hormones and pituitary hormones, and determination of the child's rate of growth. If noted, the child should be seen by a pediatric endocrinologist to consider treatment with leuprolide (Lupron) or other to slow the maturation process, delay the growth spurt, and allow greater adult height. If precocious puberty is well underway, treatment might not be possible. [Trollmann: 1998]
Sexuality and reproductive issues
When a family first hears they will have a child with spina bifida, they often have questions about fertility. Teens with spina bifida also have questions about sexuality. The usual sources of reliable information often do not address issues specific to those with physical or intellectual disabilities, leaving adolescents to feel that they are not given enough practical information. [Sawin: 2002] [Sawyer: 1999]
Although many adolescents with spina bifida are involved in intimate relationships, poor body image and fear of bowel and bladder incontinence can cause some people to limit intimate connections. [Verhoef: 2005] Adolescents with spina bifida should be taught that, like other adolescents, they may be fertile and are subject to sexually transmitted diseases. Because of the risk of latex allergy, sexually active patients should be taught to use latex-free condoms. Because the effectiveness of latex-free condoms in preventing pregnancy and sexually transmitted diseases is still being studied, males with spina bifida should use a latex-free condom inside a regular condom, and females with spina bifida should have their male partner use a latex-free condom over a regular condom. See [Walsh: 2003].
Both males and females with spina bifida may have decreased sensation in their perineal and genital regions and must watch for skin breakdown that may occur with sexual activity. Many women with spina bifida are able to become pregnant, although fertility rates aren't known. See [Jackson: 2005] for a discussion of reproductive issues in women with spina bifida. There is little information available about the sexual response in women with myelomeningocele. Adolescent females with myelomeningocele should take folic acid because of the risk of spina bifida in their children, which is greater for mothers with spina bifida than it is in the general population. See Folic Acid Supplementation & Neural Tube Defects and [Toriello: 2005].
Approximately 3/4 of males with myelomeningocele will be able to have erections, although most will experience them only from local physical stimulation rather than psychogenically. The ability to have and sustain an erection is related to the level of lesion; the lower the level, the more likely the male will be able to have an erection. Even with the ability to have an erection, many men with spina bifida will be unable to sustain it long enough for sexual intercourse. Erectile dysfunction drugs have been very helpful. If those medications fail, various surgical interventions are possible. It is unknown how many men with myelomeningocele are infertile, and whether they are infertile because they experience retrograde ejaculation or because of decreased sperm count or motility. Artificial insemination may be an option, using their own sperm. Fertility specialists should be consulted if these questions arise. [Sawin: 2002]
The medical home clinician should be prepared to address questions of sexuality if they arise in either females or males with spina bifida and might consider asking adolescents about their concerns. Some resources include [Akre: 2015], Sexually Active Woman with Spina Bifida (Spina Bifida Ireland) (
 90 KB), and Urologic and Sexual Function for Men with Spina Bifida (Spina Bifida Association) (
90 KB), and Urologic and Sexual Function for Men with Spina Bifida (Spina Bifida Association) ( 320 KB).
320 KB).
Specialty Collaborations & Other Services
Pediatric Endocrinology (see NW providers [1])
Obstetrics & Gynecology (see NW providers [0])
Pediatric Urology (see NW providers [0])
Transitions
Clinicians can find more information at Transition Resource for Individuals with Spina Bifida (Spina Bifida Association) and Transition Issues; families can find information at Navigating Transitions with Your Childand School Transitions.
Specialty Collaborations & Other Services
Social Workers (see NW providers [0])
Ask the Specialist
One of my patients has spina bifida and hydrocephalus with a shunt that has worked well for many years. Now at 14, she has headaches almost every day. She does not have nausea or vomiting. Could this be shunt related?
Most likely these headaches have nothing to do with the shunt, but she should be seen by Neurosurgery. If they feel that they are unrelated, treat like other chronic daily headaches in children. See Headache (Migraine & Chronic) for management information.
One of my patients with spina bifida gets very frequent urinary tract infections and now is starting to have impaired kidney function. Ideas?
It might be useful to bring this child and family in and review the plan for intermittent catheterization. Perhaps they are having trouble paying for supplies or having other issues in the family that are preventing adequate care.
Resources for Clinicians
On the Web
Spina Bifida Clinics (Spina Bifida Association)
A comprehensive list by state of Spina Bifida Clinics.
Care of the Child with Spina Bifida (AAP)
How primary care clinicians can improve the health and well-being of patients with spina bifida; American Academy of Pediatrics
News.
Transition Resource for Individuals with Spina Bifida (Spina Bifida Association)
Transition guidelines by age (0-18+ years old).
Helpful Articles
PubMed search for Spina Bifida in children and adolescents, last 2 years
Copp AJ, Adzick NS, Chitty LS, Fletcher JM, Holmbeck GN, Shaw GM.
Spina bifida.
Nat Rev Dis Primers.
2015;1:15007.
PubMed abstract / Full Text
Greene ND, Copp AJ.
Neural tube defects.
Annu Rev Neurosci.
2014;37:221-42.
PubMed abstract / Full Text
Burke R, Liptak GS.
Providing a primary care medical home for children and youth with spina bifida.
Pediatrics.
2011;128(6):e1645-57.
PubMed abstract
Clinical Tools
Free, printable patient education can be found for the following topics:
- Let's Talk About... Spina Bifida and Nutrition (Spanish & English)
- Let's Talk About... Hydrocephalus and Shunts (Spanish & English)
- Let's Talk About... Spina Bifida (Spanish & English)
- Let's Talk About... Spina Bifida and Bladder Control (Spanish & English)
- Let's Talk About... Clean Intermittent Catheterization for Boys (Spanish & English)
- Let's Talk About... Clean Intermittent Catheterization for Girls (Spanish & English)
- Let's Talk About... Self-Catheterization (Spanish & English)
- Let's Talk About... Spina Bifida Urologic Surgeries (Spanish & English)
Resources for Patients & Families
Information on the Web
Spina Bifida (March of Dimes)
An overview of spina bifida, which may be helpful for families with a new diagnosis.
Spina Bifida (KidsHealth)
Family-focused information about spina bifida from the Nemours Foundation.
Spina Bifida (MedlinePlus)
Information for families that includes description, frequency, causes, inheritance, other names, and additional resources;
from the National Library of Medicine.
Spina Bifida (Southwest Institute for Families &Children with Special Needs) ( 961 KB)
961 KB)
A free, 24-page booklet for teens and young adults that explains spina bifida, medical terms, diagnosis, symptoms, management,
latex precautions, and more.
National & Local Support
Spina Bifida Association
Offers programs, education, advocacy, research updates, and services nationwide. Has information and resources for all ages,
including expectant parents.
Hydrocephalus Association
An excellent resource that offers education, research, advocacy, and support to eliminate the challenges of hydrocephalus.
Studies/Registries
Spina Bifida (ClinicalTrials.gov)
Studies looking at better understanding, diagnosing, and treating this condition; from the National Library of Medicine.
Services for Patients & Families Nationwide (NW)
| Service Categories | # of providers* in: | NW | Partner states (4) (show) | | NM | NV | RI | UT | |
|---|---|---|---|---|---|---|---|---|---|
| Colorectal Care Clinics | 1 | ||||||||
| Developmental - Behavioral Pediatrics | 1 | 2 | 3 | 12 | 9 | ||||
| Dieticians and Nutritionists | 1 | 1 | 4 | 3 | 6 | ||||
| Educational Advocacy | 5 | 12 | 5 | 11 | 16 | ||||
| Food & Nutrition | 3 | 8 | 287 | 31 | 210 | ||||
| Hospitals | 3 | 11 | 23 | 14 | 57 | ||||
| Neuropsychiatry/Neuropsychology | 1 | 3 | 9 | 6 | |||||
| Obstetrics & Gynecology | 1 | 6 | 19 | ||||||
| Pediatric Endocrinology | 1 | 4 | 6 | 12 | 7 | ||||
| Pediatric Gastroenterology | 2 | 5 | 18 | 2 | |||||
| Pediatric Neurology | 5 | 5 | 18 | 8 | |||||
| Pediatric Neurosurgery | 1 | 2 | 4 | 3 | 2 | ||||
| Pediatric Ophthalmology | 1 | 6 | 6 | 8 | 4 | ||||
| Pediatric Orthopedics | 4 | 7 | 8 | 16 | 10 | ||||
| Pediatric Physical Medicine & Rehabilitation | 3 | 3 | 3 | 6 | 11 | ||||
| Pediatric Urology | 13 | 1 | 3 | ||||||
| Social Workers | 7 | 12 | |||||||
| Spina Bifida Clinics | 1 | 1 | 1 | 2 | 3 | ||||
| Vocational Education | 1 | 11 | 41 | 10 | 75 | ||||
For services not listed above, browse our Services categories or search our database.
* number of provider listings may vary by how states categorize services, whether providers are listed by organization or individual, how services are organized in the state, and other factors; Nationwide (NW) providers are generally limited to web-based services, provider locator services, and organizations that serve children from across the nation.
Authors & Reviewers
| Author: | Lynne M. Kerr, MD, PhD |
| Contributing Author: | AnnMarie Hannon, MSN, CPNP |
| Reviewer: | Betsy Ostrander, MD |
| 2013: first version: Paula Peterson, APRN, PNPA; Lynne M. Kerr, MD, PhDA; Jay Riva-Cambrin, MDA |
Bibliography
Adzick NS, Thom EA, Spong CY, Brock JW 3rd, Burrows PK, Johnson MP, Howell LJ, Farrell JA, Dabrowiak ME, Sutton LN, Gupta
N, Tulipan NB, D'Alton ME, Farmer DL.
A randomized trial of prenatal versus postnatal repair of myelomeningocele.
N Engl J Med.
2011;364(11):993-1004.
PubMed abstract
Akre C, Light A, Sherman L, Polvinen J, Rich M.
What young people with spina bifida want to know about sex and are not being told.
Child Care Health Dev.
2015;41(6):963-9.
PubMed abstract / Full Text
Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW Jr, García FA, Kemper AR, Krist AH, Kurth AE, Landefeld CS,
Mangione CM, Phillips WR, Phipps MG, Pignone MP, Silverstein M, Tseng CW.
Folic acid supplementation for the prevention of neural tube defects.
JAMA/ US Preventive Services Task Force Recommendation Statement (USPSTF).
2017;317(2):183-189.
PubMed abstract
The USPSTF recommends that all women who are planning or capable of pregnancy take a daily supplement containing 0.4 to 0.8
mg (400 to 800 µg) of folic acid.
Bowman RM, McLone DG, Grant JA, Tomita T, Ito JA.
Spina bifida outcome: a 25-year prospective.
Pediatr Neurosurg.
2001;34(3):114-20.
PubMed abstract
Bradley LA, Palomaki GE, McDowell GA.
Technical standards and guidelines: prenatal screening for open neural tube defects.
Genet Med.
2005;7(5):355-69.
PubMed abstract
Brand MC.
Part 3: examination of the newborn with closed spinal dysraphism.
Adv Neonatal Care.
2007;7(1):30-40; quiz 41-2.
PubMed abstract
An excellent discussion of the types of and significance of cutaneous markers for closed neural tube defects in babies.
Burke R, Liptak GS.
Providing a primary care medical home for children and youth with spina bifida.
Pediatrics.
2011;128(6):e1645-57.
PubMed abstract
Copp AJ, Adzick NS, Chitty LS, Fletcher JM, Holmbeck GN, Shaw GM.
Spina bifida.
Nat Rev Dis Primers.
2015;1:15007.
PubMed abstract / Full Text
Deak KL, Siegel DG, George TM, Gregory S, Ashley-Koch A, Speer MC.
Further evidence for a maternal genetic effect and a sex-influenced effect contributing to risk for human neural tube defects.
Birth Defects Res A Clin Mol Teratol.
2008;82(10):662-9.
PubMed abstract
Dupépé EB, Patel DM, Rocque BG, Hopson B, Arynchyna AA, Bishop ER, Blount JP.
Surveillance survey of family history in children with neural tube defects.
J Neurosurg Pediatr.
2017;19(6):690-695.
PubMed abstract / Full Text
Duru S, Peiro JL, Oria M, Aydin E, Subasi C, Tuncer C, Rekate HL.
Successful endoscopic third ventriculostomy in children depends on age and etiology of hydrocephalus: outcome analysis in
51 pediatric patients.
Childs Nerv Syst.
2018;34(8):1521-1528.
PubMed abstract
Edwards M, Borzyskowski M, Cox A, Badcock J.
Neuropathic bladder and intermittent catheterization: social and psychological impact on children and adolescents.
Dev Med Child Neurol.
2004;46(3):168-77.
PubMed abstract
This article describes the use of intermittent catheterization from the perspective of the individuals with myelomeningocele
and their families.
Elliott SP, Villar R, Duncan B.
Bacteriuria management and urological evaluation of patients with spina bifida and neurogenic bladder: a multicenter survey.
J Urol.
2005;173(1):217-20.
PubMed abstract
Finnell RH, Gould A, Spiegelstein O.
Pathobiology and genetics of neural tube defects.
Epilepsia.
2003;44 Suppl 3:14-23.
PubMed abstract
This is an interesting article about the embryology of NTD and the genetic and environmental contributions to NTD.
Foster, Mark M.D., Ph.D.
Spina bifida outcome: a 25-year prospective.
(2007)
http://www.emedicine.com/orthoped/topic557.htm .
Greene ND, Copp AJ.
Neural tube defects.
Annu Rev Neurosci.
2014;37:221-42.
PubMed abstract / Full Text
Jackson AB, Sipski ML.
Reproductive issues for women with spina bifida.
J Spinal Cord Med.
2005;28(2):81-91.
PubMed abstract
Jallo G, Becske T .
Neural Tube Defects.
emedicine; (2005)
http://www.emedicine.com/neuro/topic244.htm.
Juriloff DM, Harris MJ.
Hypothesis: the female excess in cranial neural tube defects reflects an epigenetic drag of the inactivating X chromosome
on the molecular mechanisms of neural fold elevation.
Birth Defects Res A Clin Mol Teratol.
2012;94(10):849-55.
PubMed abstract
Kancherla V, Wagh K, Johnson Q, Oakley GP Jr.
A 2017 global update on folic acid-preventable spina bifida and anencephaly.
Birth Defects Res.
2018.
PubMed abstract
Kaufman BA.
Neural tube defects.
Pediatr Clin North Am.
2004;51(2):389-419.
PubMed abstract
Interesting article regarding the embryology of NTD. This article also points out that NTDs are not progressive and any deterioration
should prompt evaluation and treatment.
King JC, Currie DM, Wright E.
Bowel training in spina bifida: importance of education, patient compliance, age, and anal reflexes.
Arch Phys Med Rehabil.
1994;75(3):243-7.
PubMed abstract
A description of some toileting interventions for individuals with spina bifida.
Klepper J, Busse M, Strassburg HM, Sorensen N.
Epilepsy in shunt-treated hydrocephalus.
Dev Med Child Neurol.
1998;40(11):731-6.
PubMed abstract
Lee NG, Gomez P, Uberoi V, Kokorowski PJ, Khoshbin S, Bauer SB, Estrada CR.
In utero closure of myelomeningocele does not improve lower urinary tract function.
J Urol.
2012;188(4 Suppl):1567-71.
PubMed abstract
Liptak, G.S.
Evidence-based Practice in Spina Bifida: Developing A Research Agenda.
Evidence-based Practice in Spina Bifida, 2003; Washington D.C..
/ http://web.archive.org/web/20040701175406/http://www.sbaa.org/site/Doc...
Lollar, D.J.
Learning Among Children with Spina Bifida.
Spina Bifida Spotlight. 1995;
This article describes learning problems and possible interventions in children with myelomeningocele.
Marreiros H, Loff C, Calado E.
Osteoporosis in paediatric patients with spina bifida.
J Spinal Cord Med.
2012;35(1):9-21.
PubMed abstract / Full Text
Meyer S, Landau H.
Precocious puberty in myelomeningocele patients.
J Pediatr Orthop.
1984;4(1):28-31.
PubMed abstract
Mulholland CB, Aranda G, Arredondo LA, Calgua E, Contreras F, Espinoza DM, Gonzalez JB, Hoil JA, Komolafe E, Lazareff JA,
Liu Y, Soto-Mancilla JL, Mannucci G, Nan B, Portillo S, Zhao H.
The International Tethered Cord Partnership: Beginnings, process, and status.
Surg Neurol Int.
2011;2:38.
PubMed abstract / Full Text
National Center on Birth Defects and Developmental Disabilities.
Data & Statistics on Spina Bifida.
Centers for Disease Control and Prevention; (2019)
https://www.cdc.gov/ncbddd/spinabifida/data.html. Accessed on Dec. 2019.
Noetzel MJ, Blake JN.
Prognosis for seizure control and remission in children with myelomeningocele.
Dev Med Child Neurol.
1991;33(9):803-10.
PubMed abstract
Proos LA, Dahl M, Ahlsten G, Tuvemo T, Gustafsson J.
Increased perinatal intracranial pressure and prediction of early puberty in girls with myelomeningocele.
Arch Dis Child.
1996;75(1):42-5.
PubMed abstract / Full Text
Pruitt LJ.
Living with spina bifida: a historical perspective.
Pediatrics.
2012;130(2):181-3.
PubMed abstract / Full Text
Sawin, K.J., Buran, C.F., Brei, T.J., and Fastenau, P.S.
Sexuality Issues in Adolescents with A Chronic Neurological Condition.
J. Perinat. Educ.
2002;11(1):22-34.
Sawyer SM, Roberts KV.
Sexual and reproductive health in young people with spina bifida.
Dev Med Child Neurol.
1999;41(10):671-5.
PubMed abstract
Sgouros S, Kulkharni AV, Constantini S.
The international infant hydrocephalus study: concept and rational.
Childs Nerv Syst.
2006;22(4):338-345.
PubMed abstract
Shin M, Kucik JE, Siffel C, Lu C, Shaw GM, Canfield MA, Correa A.
Improved survival among children with spina bifida in the United States.
J Pediatr.
2012;161(6):1132-7.
PubMed abstract
Spina Bifida Association.
Guidelines for the management of spina bifida.
2018; https://www.spinabifidaassociation.org/guidelines/
This 4th edition is evidence based, where evidence exists, and otherwise based on expert opinion. It includes 25 topics for
care of the individual with spina bifida from birth through adulthood. Recent additions include an emphasis on coordination
of care, multidisciplinary care, and culturally sensitive care.
Sufianov AA, Sufianova GZ, Iakimov IA.
Endoscopic third ventriculostomy in patients younger than 2 years: outcome analysis of 41 hydrocephalus cases.
J Neurosurg Pediatr.
2010;5(4):392-401.
PubMed abstract
Talwar D, Baldwin MA, Horbatt CI.
Epilepsy in children with meningomyelocele.
Pediatr Neurol.
1995;13(1):29-32.
PubMed abstract
Toriello HV.
Folic acid and neural tube defects.
Genet Med.
2005;7(4):283-4.
PubMed abstract
Trivedi J, Thomson JD, Slakey JB, Banta JV, Jones PW.
Clinical and radiographic predictors of scoliosis in patients with myelomeningocele.
J Bone Joint Surg Am.
2002;84-A(8):1389-94.
PubMed abstract
Trollmann R, Strehl E, Dorr HG.
Precocious puberty in children with myelomeningocele: treatment with gonadotropin-releasing hormone analogues.
Dev Med Child Neurol.
1998;40(1):38-43.
PubMed abstract
Verhoef M, Barf HA, Vroege JA, Post MW, Van Asbeck FW, Gooskens RH, Prevo AJ.
Sex education, relationships, and sexuality in young adults with spina bifida.
Arch Phys Med Rehabil.
2005;86(5):979-87.
PubMed abstract
Verpoorten C, Buyse GM.
The neurogenic bladder: medical treatment.
Pediatr Nephrol.
2008;23(5):717-25.
PubMed abstract / Full Text
Vogel TW, Bahuleyan B, Robinson S, Cohen AR.
The role of endoscopic third ventriculostomy in the treatment of hydrocephalus.
J Neurosurg Pediatr.
2013;12(1):54-61.
PubMed abstract
Walsh TL, Frezieres RG, Peacock K, Nelson AL, Clark VA, Bernstein L.
Evaluation of the efficacy of a nonlatex condom: results from a randomized, controlled clinical trial.
Perspect Sex Reprod Health.
2003;35(2):79-86.
PubMed abstract
Warf BC, Campbell JW.
Combined endoscopic third ventriculostomy and choroid plexus cauterization as primary treatment of hydrocephalus for infants
with myelomeningocele: long-term results of a prospective intent-to-treat study in 115 East African infants.
J Neurosurg Pediatr.
2008;2(5):310-6.
PubMed abstract
Webb HW, Barraza MA, Stevens PS, Crump JM, Erhard M.
Bowel dysfunction in spina bifida--an American experience with the ACE procedure.
Eur J Pediatr Surg.
1998;8 Suppl 1:37-8.
PubMed abstract
Williams J, Mai CT, Mulinare J, Isenburg J, Flood TJ, Ethen M, Frohnert B, Kirby RS.
Updated estimates of neural tube defects prevented by mandatory folic Acid fortification - United States, 1995-2011.
MMWR Morb Mortal Wkly Rep.
2015;64(1):1-5.
PubMed abstract / Full Text
Wong LY, Paulozzi LJ.
Survival of infants with spina bifida: a population study, 1979-94.
Paediatr Perinat Epidemiol.
2001;15(4):374-8.
PubMed abstract
Yerby MS.
Teratogenicity and antiepileptic drugs: potential mechanisms.
Int Rev Neurobiol.
2008;83:181-204.
PubMed abstract
Yoshida F, Morioka T, Hashiguchi K, Kawamura T, Miyagi Y, Nagata S, Mihara F, Ohshio M, Sasaki T.
Epilepsy in patients with spina bifida in the lumbosacral region.
Neurosurg Rev.
2006;29(4):327-32; discussion 332.
PubMed abstract

