Calcium & Vitamin D
Calcium and vitamin D are critical to bone health, especially in children. Children and youth with special health care needs (CYSHCN) may be at increased risk for nutritional deficiencies and bone-related problems like Osteoporosis and Pathologic Fractures. This page discusses when and how to test calcium and vitamin D levels and to counsel families regarding dietary intake and supplementation.
Dietary Recommendations
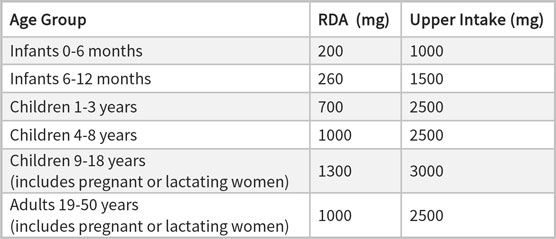
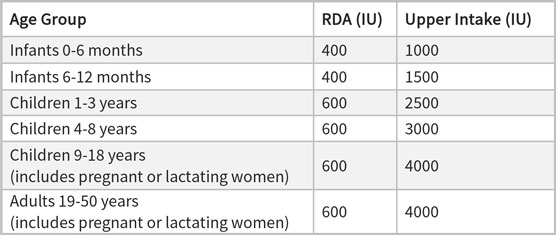
The American Academy of Pediatrics (AAP) and other health experts recommend that children get their nutrients from a healthy diet. Intake recommendations often contain the following terms:
- Recommended daily allowances (RDA) - the average daily dietary intake levels needed to meet the nutritional needs of most people
- Adequate intake - a term used instead of RDA when there is less evidence for the daily dietary intake likely needed for adequate nutrition
- Upper intake - the limit of routine dietary intake above which most people might be at risk for toxicity, though higher intake may still be indicated for people with unusual needs
Calcium Dietary Intake Recommendations
Vitamin D Dietary Intake Recommendations
Dietary Sources of Calcium
- Milk: An 8-oz glass of cow milk contains about 300 mg of calcium (for lactose-intolerant individuals, tolerance may be improved with use of lactose-free dairy products or lactase enzymes).
- Yogurt: An 8-oz serving of plain yogurt contains about 275 mg of calcium.
- Cheese: A 1.5-oz serving of cheese contains about 300 mg of calcium.
Dietary Sources of Vitamin D
- Fatty fish (sardines, salmon, tuna, and cod liver oil): A 3.5-oz serving of fresh, wild-caught salmon contains about 1,000 IU of vitamin D (farmed salmon has about 1/8th the amount of vitamin D).
- Shitake mushrooms: A 3.5-oz serving of canned shitake mushrooms provides about 1,600 IU of vitamin D.
- Fortified fruit juices, formulas, cereals, and dairy products: An 8-oz serving of cow milk or baby formula, fortified orange juice, yogurt, or a 3-oz serving of cheese has about 100 IU of vitamin D.
- Eggs: A hard-boiled egg contains about 20 IU of vitamin D.
Breastfed infants do not get the recommended 400 IU of vitamin D daily unless supplemented; typically, breastmilk contains about 20-25 IU/L. [Institute: 2011]
Pearls and Alerts
Risks Factors
Despite consumption of recommended amounts of calcium and vitamin D, children and youth with special health needs may be at
risk for deficiencies due to their medical condition, medications, activity level, etc. Risk factors are discussed in more
detail in the Portal's Osteoporosis and Pathologic Fractures.
Risk of Overdose
Children are at risk of toxic ingestion of nutritional supplements and may be particularly tempted by tasty chewable formulations
(e.g., gummies).
Iron Interacts with Calcium
Calcium ingested at the same time as iron can reduce iron absorption.
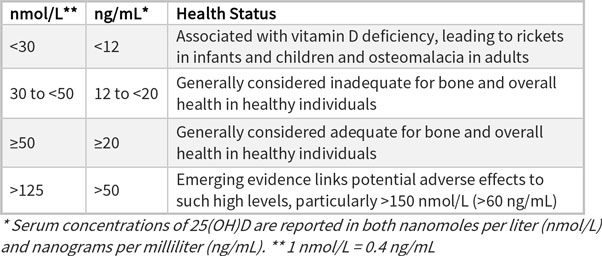
Testing Calcium and Vitamin D Levels
Calcium
Vitamin D
Supplementation
For nutritionally vulnerable populations or children who do not meet the RDA with their diet, vitamin and mineral supplements may help meet nutrition needs. Because supplements are not regulated, quality may vary and it is difficult to recommend specific formulations.
Calcium Supplementation
Calcium supplementation (often combined with vitamin D) may be considered for children who have significantly inadequate dietary intake or risk for poor bone health. There is “possible benefit” from supplementing calcium and vitamin D in children with cerebral palsy to increase bone density, but insufficient evidence to show supplementation helps prevent fragility fractures. [Ozel: 2016]Risks of excess calcium supplementation include increased calcium excretion in the urine (which can lead to kidney stones), muscle cramping, bone problems, neurological problems, and heart attack and strokes in older people.
Vitamin D Supplementation

- Oral/enteral supplement for the infant with 400 IU daily of vitamin D (most commonly recommended)
- Oral supplement for the mothers with 6,000 IU daily to provide adequate vitamin D in the breastmilk
Resources
Information & Support
For Professionals
Vitamin D: Fact Sheet for Health Professionals (NIH)
Guidelines and information about sources of vitamin D, its potential interactions with medications, what constitutes excessive
amounts, and who is at risk for deficiencies; National Institutes of Health.
Calcium: Fact Sheet for Health Professionals (NIH)
Guidelines and information about sources of calcium, its potential interactions with medications, lactose intolerance, and
who is at risk for deficiencies; National Institutes of Health.
Dietary Guidelines for Americans 2015-2020 (HHS & USDA)
Details about healthy eating patterns, limiting calories from added sugars and saturated fats, reducing sodium intake, and
shifting to healthier food and beverage choices; U.S. Dept. of Health and Human Services and U.S. Dept. of Agriculture.
Vitamin D and Breastfeeding (CDC)
Information about breast milk and vitamin D content; Centers for Disease Control and Prevention.
For Parents and Patients
Calcium Content of Foods (UCSF)
List of foods, serving sizes, and amounts of calcium (mg); University of California San Francisco.
Food Sources of Vitamin D (Dietitians of Canada)
List of foods, serving sizes, and amounts of vitamin D (IU).
Vitamin D and Your Child (JAMA)
One-page overview focused on children without special needs; JAMA Pediatrics.
Calcium: Fact Sheet for Consumers (NIH)
Learn about the importance of calcium, where to find it in foods and supplements, how much is needed, and how much is too
much; National Institutes of Health.
Vitamin D: Fact Sheet for Consumers (NIH)
Learn about the importance of vitamin D, where to find it in foods and supplements, how much is needed, and how much is too
much; National Institutes of Health.
Calcium: Fact Sheet for Consumers in Spanish (NIH)
Learn about the importance of calcium, where to find it in foods and supplements, how much is needed, and how much is too
much; National Institutes of Health.
Vitamin D: Fact Sheet for Consumers in Spanish (NIH)
Learn about the importance of vitamin D, where to find it in foods and supplements, how much is needed, and how much is too
much; National Institutes of Health.
Helpful Articles
Golden NH, Abrams SA.
Optimizing bone health in children and adolescents.
Pediatrics.
2014;134(4):e1229-43.
PubMed abstract / Full Text
Authors & Reviewers
| Authors: | Jennifer Goldman, MD, MRP, FAAP |
| Elizabeth Miller, MS, RD |
| 2018: update: Jennifer Goldman, MD, MRP, FAAPA |
| 2015: update: Meghan S Candee, MD, MScCA; Elizabeth Miller, MS, RDCA |
| 2013: first version: Lynne M. Kerr, MD, PhDA |
Page Bibliography
Golden NH, Abrams SA.
Optimizing bone health in children and adolescents.
Pediatrics.
2014;134(4):e1229-43.
PubMed abstract / Full Text
Heaney RP.
Vitamin D in health and disease.
Clin J Am Soc Nephrol.
2008;3(5):1535-41.
PubMed abstract / Full Text
Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium; Ross AC, Taylor CL, Yaktine
AL, Del Valle HB, editors.
Dietary Reference Intakes for Calcium and Vitamin D.
The National Academies Collection: Reports funded by National Institutes of Health.
2011.
PubMed abstract / Full Text
Maguire JL, Lebovic G, Kandasamy S, Khovratovich M, Mamdani M, Birken CS, Parkin PC.
The relationship between cow's milk and stores of vitamin D and iron in early childhood.
Pediatrics.
2013;131(1):e144-51.
PubMed abstract
National Institutes of Health.
Dietary Supplement Ingredient Database.
(2018)
http://dsid.od.nih.gov/. Accessed on April 2019.
Ozel S, Switzer L, Macintosh A, Fehlings D.
Informing evidence-based clinical practice guidelines for children with cerebral palsy at risk of osteoporosis: an update.
Dev Med Child Neurol.
2016;58(9):918-23.
PubMed abstract
Russo S, Carlucci L, Cipriani C, Ragno A, Piemonte S, Fiacco RD, Pepe J, Fassino V, Arima S, Romagnoli E, Minisola S.
Metabolic Changes Following 500 μg Monthly Administration of Calcidiol: A Study in Normal Females.
Calcif Tissue Int.
2011.
PubMed abstract
University of Iowa.
Pediatric reference ranges common hematology and chemistry tests.
(2018)
https://www.healthcare.uiowa.edu/path_handbook/Appendix/Heme/PEDIATRIC.... Accessed on April 2019.
Winzenberg T, Powell S, Shaw KA, Jones G.
Effects of vitamin D supplementation on bone density in healthy children: systematic review and meta-analysis.
BMJ.
2011;342:c7254.
PubMed abstract / Full Text
Zaniew M, Jarmoliński T.
Vitamin D status and bone density in steroid-treated children with glomerulopathies: effect of cholecalciferol and calcium
supplementation.
Adv Med Sci.
2012;57(1):88-93.
PubMed abstract