Asthma
Overview

Current published guidelines for asthma care include: The differences between them will be addressed where needed below.
Other Names & Coding
J45.2x, Mild intermittent asthma
J45.3x, Mild persistent asthma
J45.4x, Moderate persistent asthma
J45.5x, Severe persistent asthma
J45.9xx, Other and unspecified asthma
The x indicates that an additional digit is required. ICD-10 Asthma Coding Reference (icd10data.com) provides details.
Prevalence
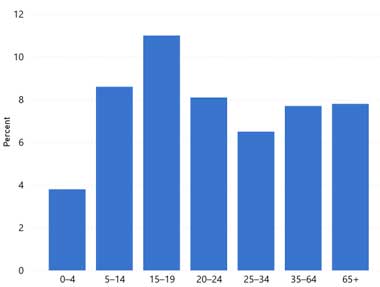
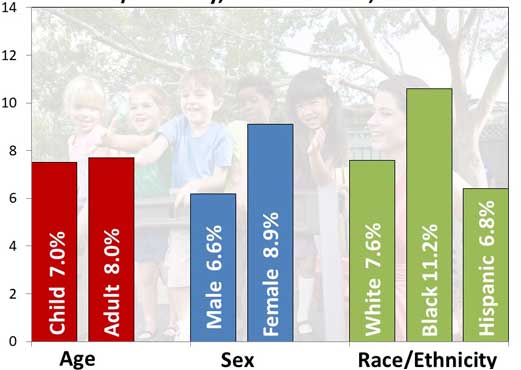
| Prevalence of Asthma in the United States by Age | Asthma Prevalence by Age, Sex, Race/Ethnicity |
Genetics
Prognosis
Practice Guidelines
National Asthma Education and Prevention Program Expert Panel.
Expert Panel Report 3 (EPR3): Guidelines for the Diagnosis and Management of Asthma.
National Heart Lung and Blood Institute, NIH; (2007)
https://www.nhlbi.nih.gov/health-topics/guidelines-for-diagnosis-manag.... Accessed on 6/24/2021.
For the full 440-page report, click the Download PDF 4 MB button; from the National Heart Lung and Blood Institute, National
Institutes of Health. A 60-page Summary Report and a 12-page Asthma Care Quick Reference are also downloadable from the same
web page.
Cloutier MM, Baptist AP, Blake KV, Brooks EG, Bryant-Stephens T, DiMango E, Dixon AE, Elward KS, Hartert T, Krishnan JA, Lemanske
RF Jr, Ouellette DR, Pace WD, Schatz M, Skolnik NS, Stout JW, Teach SJ, Umscheid CA, Walsh CG.
2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program
Coordinating Committee Expert Panel Working Group.
J Allergy Clin Immunol.
2020;146(6):1217-1270.
PubMed abstract / Full Text
Reddel HK et al.
2021 GINA Report, Global Strategy for Asthma Management and Prevention.
Global Initiative for Asthma.
2021.
/ https://ginasthma.org/gina-reports/
A downloadable 217-page report with guidelines for the care of children (and adults) with asthma from the World Health Organization.
A "What's New in 2021" report. GINA does not distinguish between mild persistent asthma and intermittent asthma.
Roles of the Medical Home
Clinical Assessment
Overview
Pearls & Alerts for Assessment
Spirometry in childrenObtaining accurate spirometry in children, especially those under 5 years of age, can be difficult. Seek the most experienced available resource when spirometry is needed for younger patients. If performing spirometry in a primary care setting, assure reliable flow-volume loops. Spirometry360 provides a training program for office staff that involves distance verification of reliability.
Peak flow monitoringPeak flow meters may be helpful for children ages 6 and older with moderate to severe persistent asthma who require daily asthma medications. It is most helpful when used and tracked daily around the same time of the day. Daily readings help families to recognize early drops in airflow (peak expiratory flow (PEF) < 80% of personal best). Of note, children’s personal best improves with growth.
Short-acting beta-agonists (SABAs)Frequent use of short-acting beta-agonists (SABAs), particularly SABA nebulizers, in the past 3 months is associated with poor asthma outcomes, such as asthma-related Emergency Department visits and asthma-related hospitalizations. [Paris: 2008]
Screening
Presentations
Typical symptoms include:
- History of:
- Cough, particularly at night or after activities/exercise, with or without wheezing
- Recurrent wheezing
- Recurrent difficulty in breathing or chest tightness
- Triggered or worsening with:
- Sleep, awakening patient (and family)
- Exercise/activities
- Viral infection
- Inhalant allergens (e.g., animals with fur or hair, house-dust mites, mold, pollen)
- Irritants (tobacco or wood smoke, airborne chemicals)
- Changes in weather
- Strong emotional expression (laughing or crying hard)
- Stress
- Menstrual cycles
- Rapid breathing
- Sighing
- Fatigue, inability to exercise properly
- Difficulty sleeping
- Anxiety, difficulty concentrating
- Upper airway noises, such as stertor, stridor, or snoring
Cough variant asthma (CVA) occurs in all ages but may be over-diagnosed in children. Probably no more than 5% of asthmatic children have cough as the only or primary symptom, and the cough should resolve with appropriate asthma medications and recur when the medications are stopped. [Kercsmar: 2019]
Diagnostic Criteria
- Symptoms of recurrent airway obstruction or airway hyperresponsiveness, which can be usually linked to a trigger (e.g., viral infection)
- Airway obstruction that is at least partially reversible
- Alternative diagnoses have been excluded, which may require additional studies
Clinical Classification
- Intermittent
- Mild persistent
- Moderate persistent
- Severe persistent
- Well-controlled
- Not well-controlled
- Very poorly controlled
 59 KB).
59 KB).
Differential Diagnosis
The following differential diagnoses are from the NHLBI Guidelines. [National: 2007]
- Vascular rings or laryngeal webs
- Upper airway disease
- Allergic rhinitis and sinusitis
- Foreign body in trachea or bronchus
- Obstruction involving large airways
- Paradoxical vocal fold motion (previously referred to as vocal cord dysfunction)
- Laryngotracheomalacia, tracheal stenosis, or bronchostenosis
- Enlarged lymph nodes or tumor
- Obstructions involving small airways
- Viral bronchiolitis
- Cystic fibrosis
- Bronchopulmonary dysplasia
- Heart disease
- Other causes
- Recurrent cough, not due to asthma
- Aspiration from swallowing mechanism dysfunction or gastroesophageal reflux
Comorbid & Secondary Conditions
Rhinosinusitis, relatively common in children with atopy, may trigger and/or exacerbate asthma symptoms. Patients with nasal polyposis and asthma are likely to have aspirin-exacerbated respiratory disease (AERD). Those patients may have sudden, life-threatening flares of asthma after ingestion of aspirin or non-steroidal anti-inflammatory drugs (NSAIDs).
Vocal cord dysfunction (VCD, also called paradoxical vocal fold motion or inducible laryngeal obstruction) can exist by itself (in the differential diagnosis for exercise-induced asthma) or coexist with asthma. VCD is more common in female adolescents participating in competitive sports, especially those with a history of anxiety. VCD symptoms can be triggered by uncontrolled rhinosinusitis and/or GERD.
Depression, anxiety, behavioral problems, and learning disabilities are common among children with asthma. [University: 2013] An association among asthma and internalizing disorders in children, such as panic disorder, social phobia, separation anxiety, and generalized anxiety, has been observed. [Carrera-Bojorges: 2013] See Depression and Anxiety Disorders for treatment details.
Obstructive sleep apnea and asthma are highly prevalent respiratory disorders and are frequently comorbid. Risk factors common to the 2 diseases include obesity, rhinitis, and gastroesophageal reflux. [Prasad: 2013]
Children who are obese or overweight are 1.16 to 1.37 times more likely to develop asthma than normal-weight kids; the risk grows as their body-mass index increases. Obese children also experience more frequent and severe episodes of asthma, requiring more medical attention and drug therapy. [Oxford: 2013] See Missing link with id: 99e6f817.xml for treatment details.
History & Examination
- Assessment of asthma severity/control to guide therapeutic decisions
- Understanding the impact of asthma on the child and family to guide the accessing of needed resources and/or accommodations in the school or community
 57 KB) offers a comprehensive list.
57 KB) offers a comprehensive list.
Current & Past Medical History
Pattern of symptoms: Perennial, seasonal, or both; continual, episodic, or both; onset, duration, frequency, diurnal variations, especially nocturnal, upon awakening, or with exercise
Precipitating and/or aggravating factors: Symptoms of comorbid conditions, such as reflux, viral exposures, allergens, home characteristics
Disease course: Age at onset, progression, current management, frequency of using short-acting beta2-agonist (SABA), oral corticosteroids, current Asthma Action Plan
History of exacerbations: Usual prodromal signs and symptoms, rapidity of onset, duration, frequency, need for urgent or emergent care, hospitalization, intensive care unit admission, limitations to physical activity, exertion, play, exercise, sleep
Comorbid conditions: Gastroesophageal reflux, obesity, obstructive sleep apnea, rhinitis or sinusitis, stress, and depression, or allergic bronchopulmonary aspergillosis
Current medications: Frequency and technique, complementary and alternative medications, reasons for not using prescribed medications (inadequate technique and/or adherence are very common)
Medication side effects: Headache, sleeplessness, nausea, nervousness/tremors, thrush, and behavioral changes
The Asthma Control Test (ACT) is a validated assessment tool that provides a score for recent asthma symptoms. Scores of 19 or below suggest suboptimal control.
- The Asthma Control Test for Children & Adults (asthma.com) provides online fillable ACTs.
- The Asthma Control Test for Children 4-11 Years Old (GlaxoSmithKline) (
 ) and Asthma Control Test for People 12 Years or Older (GlaxoSmithKline) (
) and Asthma Control Test for People 12 Years or Older (GlaxoSmithKline) ( 138 KB) are downloadable PDF versions.
138 KB) are downloadable PDF versions.
Pregnancy/Perinatal History
Developmental & Educational Progress
How is school performance affected by asthma symptoms or medications? Is the child able to fully participate in sports and physical education?
Does the student have an active health plan at school and rescue medications available?
Does the student have or need a 504 Plan or other accommodations?
Social & Family Functioning
Ask about the impact of asthma on the patient and family, including the episodes of unscheduled care (emergency department, urgent care, hospitalization); number of days missed from school/work; limitations of activity, especially sports and strenuous work; history of nocturnal awakening; effect on growth, development, behavior, school or work performance, and lifestyle; impacts on family routines, activities, or dynamics; and economic impact. Have there been problems with family adjustment to asthma?
Enquire about the patient's and family's perceptions of disease, including knowledge of asthma and treatment and beliefs or concerns regarding the use and long-term effects of medications; the ability of the patient and parents to cope with disease and recognize severity of an exacerbation; the level of family support; economic resources; and sociocultural beliefs.
Physical Exam
Vital Signs
Growth Parameters
Height and weight (current and patterns of gain) for evidence of other chronic underlying diseases (e.g., cystic fibrosis), effect of medications, obesity (might complicate asthma)
HEENT/Oral
Evidence of allergy (periorbital swelling, conjunctival injection or edema, nasal discharge, nasal polyps, pale or swollen nasal turbinates, Dennie-Morgan lines, mouth breathing), sinusitis, otitis media, or effusion
Testing
Laboratory Testing
Imaging
Genetic Testing
Other Testing
Spirometry: Spirometry should be performed in children ≥5 years to assess airflow obstruction and reversibility with treatment. Spirometry should be repeated 1) after treatment has resulted in symptom control to document attainment of (near) normal airway function, 2) when symptoms seem poorly controlled, to evaluate causes, and 3) every 1-2 years to detect decreasing control or decline in pulmonary function over time. [National: 2007] In children, optimal technique is crucial for obtaining accurate results. One study found more than 3/4 of spirometries in primary care pediatric clinics were unacceptable. [Gillette: 2011] For children <5 years, spirometry may be attempted, but it may not be reliable.
Peak flow: Although there is less emphasis on peak expiratory flow measurement in recent guidelines, these measurements are still widespread. Taking peak flow measurements is quick, easy, inexpensive, and, with practice, it can be sufficiently reliable to guide daily therapy or in-office assessment. After initial diagnosis, peak flow measurements can be used to monitor response to treatment.
Understanding the intricacies of peak flow use helps achieve more accurate readings:
- They are extremely effort-dependent.
- Personal best, rather than predicted value, should be used as the 100% value.
- Many children cannot perform an adequate peak flow maneuver.
- Personal best increases with height (as do predicted values).
- They are not as sensitive in children as FEV1 or FEF 25-75% (mean forced expiratory flow between 25% to 75% of the FVC) for assessing airflow obstruction.
Methacholine challenge: The methacholine bronchoprovocation challenge is for assessing lower airway hyperreactivity. If the diagnosis of asthma is uncertain, most notably when spirometry performed before and after bronchodilator has not established or eliminated the diagnosis, a methacholine challenge testing may be used. Optimal diagnostic value of the test occurs when the pretest probability of asthma is 30-70%. Of note, it is more useful in excluding a diagnosis of asthma than in establishing one. [Crapo: 2000]
Fractional Exhaled Nitric Oxide (FeNO): FeNO is a measure of eosinophilic airway inflammation and is recommended for patients older than 5 years for whom the diagnosis of asthma remains uncertain following history, physical exam, and spirometry or for those unable to complete spirometry. FeNO testing should not be used alone to diagnose asthma. The test is not recommended for children 0-4 years and it can be normal in some patients with asthma. FeNO levels greater than 50 ppb in patients over 12 years (>35 ppb in those 5-12 years) are consistent with elevated T2 inflammation and support a diagnosis of asthma. While FeNO is frequently elevated in patients with asthma, it may also be elevated in other non-asthma atopic conditions; low FeNO levels (<20 ppb in children) can be found in a variety of non-asthma pulmonary conditions. The use of FeNO may help identify asthma subtypes and predict responses to therapy. For more detailed recommendations, see 2020 Clinician's Guide - FeNO Testing (NHLBI) (
 360 KB). FeNO testing is
typically performed in asthma centers and by clinics that see a lot of asthma patients.
360 KB). FeNO testing is
typically performed in asthma centers and by clinics that see a lot of asthma patients.Exercise challenge: If necessary for diagnosis, an exercise challenge with PEF or FEV1 measurements before, at 5-minute intervals during, and following a 20- to 30-minute exercise period may be performed. The test is considered positive if either measure declines by 15% or more.
Specialty Collaborations & Other Services
Pulmonary Function Testing (see NW providers [0])
Pediatric Pulmonology (see NW providers [0])
Pediatric Allergy (see NW providers [1])
Treatment & Management
Overview
-
2020 Focused Updates to the Asthma Management Guidelines
Expert Panel Report 4 (NHLBI) Working Group, of the National Heart, Lung,
and Blood Institute (NHLBI)
- The NHLBI 2020 Report updates the previous 2007 EPR-3 regarding 6 key topics based on review of literature published before 2016. [Cloutier: 2020]
-
2021 Global Initiative for Asthma (GINA), a
collaboration among the NHLBI and the World Health Organization (WHO), which
is updated yearly.
- GINA does not distinguish between mild persistent asthma and intermittent asthma but the NHLBI 2020 Report does.
- In the 2021 GINA, for ongoing treatment, 2 tracks for management for adolescents and adult are described. Track 1 (the preferred approach) - with low-dose ICS-LABA as reliever therapy. Track 2 with SABA as the reliever as the alternative approach if Track 1 is not possible, or not preferred, by a patient with no exacerbations on their current therapy. [Reddel: 2021]
Flow of Asthma Care
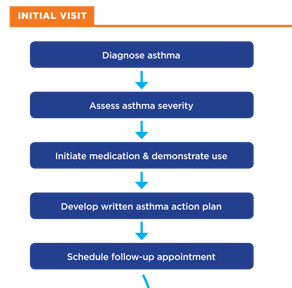 |
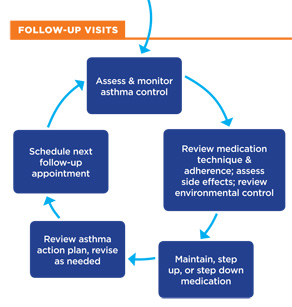 |
| Image adapted from [National: 2007] |
Referral to a specialist in asthma care (comprehensive asthma program/clinic, pediatric pulmonology, or pediatric allergy, depending on local availability) is recommended if:
- Patient has a history of hospitalization or ICU stay for asthma exacerbation.
- Asthma is uncontrolled after 3-5 months of treatment; patient required >2 courses of oral corticosteroids in 1 year.
- Asthma signs and symptoms are atypical, and other diagnoses are considered (e.g., sinusitis, nasal polyps, allergic bronchopulmonary aspergillosis (ABPA), paradoxical vocal fold motion, gastroesophageal reflux disease (GERD), chronic obstructive pulmonary disease (COPD).
- Additional testing is considered, such as allergy skin prick testing, lung function testing, imaging, or evaluation via bronchoscopy.
- Patient requires additional education and guidance about the complications of therapy, problems with adherence, or allergen avoidance.
- Patient is being considered for immunotherapy.
- Patient has at least moderate persistent asthma (Step 3 for children 0-4 years of age, Step 4 for 5+ years; consider referral for Step 2 in children 0-4 years of age).
Programs/clinics that focus on comprehensive asthma care have been shown to significantly reduce emergency department visits, hospitalizations, and missed school days. [Weinberger: 2016]
Pearls & Alerts for Treatment & Management
Inhaler skills and adherenceMost patients (up to 80%) cannot use their inhaler correctly. At least 50% of adults and children do not take controller medications as prescribed. [Reddel: 2021]
Use of single maintenance and reliever therapy (SMART)Use of a combination form of inhaled corticosteroid (ICS) and long-acting beta2-agonist (LABA, formoterol) is recommended for patients 4 years and older with a history of a severe exacerbation in the past 12 months. ICS-formoterol should not be used in those taking ICS-salmeterol for maintenance therapy.
Long-acting muscarinic antagonists (LAMA)LAMA are recommended for patients 12-years or older with uncontrolled persistent asthma but should not be used in those with urinary retention or glaucoma.
AllergiesTreatment of allergic rhinitis and chronic rhinosinusitis reduces nasal symptoms but does not improve asthma control. [Reddel: 2021]
Food allergiesConfirmed food allergy is a risk factor for asthma-related death. Patients with asthma and food allergies should have an anaphylaxis plan and be trained in avoidance strategies and use of injectable epinephrine. [Reddel: 2021]
ObesityPatients with obesity and asthma have more difficult-to-control asthma due to comorbid pro-inflammatory conditions. Asthma complicates obesity care; asthma flares often require patients to take oral corticosteroids, which may lead to increased appetite and weight gain. Weight reduction, even by 5-10%, can improve asthma control. [Reddel: 2021]
SurgeryWell-managed asthma reduces potential complications of surgery. Optimize control prior to surgery, including using a short course of oral corticosteroids if needed. [National: 2007]
PregnancyOne-third of women during pregnancy have asthma worsen, and 1/3 of pregnant women have asthma improve - medications should be adjusted accordingly. Maintaining lung function helps ensure oxygen supply to the fetus. Inhaled corticosteroids (ICS) are preferred for long-term control. [National: 2007] Budesonide is the preferred ICS because more data are available on this medication during pregnancy. [National: 2007]
DepressionFor children with asthma, treatment for comorbid depression increases compliance and improves outcomes. Early recognition may allow intervention before significant symptoms develop. In cases of severe asthma, treatment of depression may also decrease mortality. [Galil: 2000]
Neuropsychiatric complicationsNeuropsychiatric events have been reported in some patients taking montelukast (Singulair), zafirlukast (Accolate), and zileuton (Zyflo and Zyflo CR). The Food and Drug Administration has requested that manufacturers include a precaution in the drug prescribing information. Reported neuropsychiatric events include post-market cases of agitation, aggression, anxiousness, dream abnormalities, hallucinations, depression, insomnia, irritability, restlessness, suicidal thinking and behavior (including suicide), and tremor.
How should common problems be managed differently in children with Asthma?
Growth or Weight Gain
Viral Infections
Over the Counter Medications
Systems
Respiratory
The table below summarizes the age-based classification of asthma severity and initiation of treatment. Components of severity include impairment (reduction in lung function, frequency of symptoms, daily activity limitations, frequency of night awakenings, and medication use if pertinent) and risk (frequency and intensity of exacerbations).
Classifying Asthma Severity and Initiating Therapy
 |
Click on the image to download a PDF of the table
from the 2007 Asthma Care Quick Reference (EPR-3) ( 719 KB). 719 KB).
|
The table below can guide the assessment of asthma control and changes in treatment during follow-up visits. Assessment of control is based on impairment and risk. Components of impairment include frequency of nighttime awakenings, SABA use, normal activity interruptions, lung function, and validated questionnaire scores (e.g., the Asthma Control Test - questionnaires for various ages can be found at Asthma). Components of risk include exacerbations, corticosteroid use, lung health, and side-effects of treatment.
Assessing Asthma Control & Adjusting Therapy
 |
Click on the image to download a PDF of the table
from the 2007 Asthma Care Quick Reference (EPR-3) ( 719 KB). 719 KB).
|
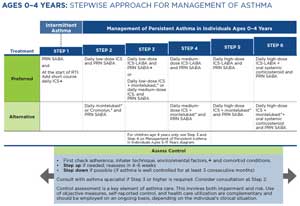
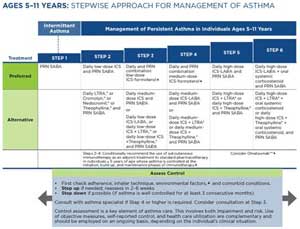
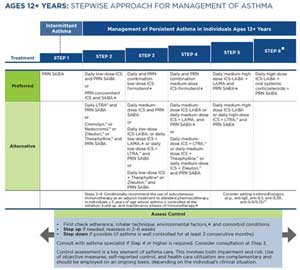
Ongoing treatment: The 2020 Focused Updates to the NHLBI Guidelines describe “Six Steps” in treatment for asthma based on severity (prior to treatment) or control (on treatment). The management for each step varies somewhat by age group: 0-4 years, 5-11 years, and 12 years and older. In a child with poorly controlled asthma, stepping up to the next treatment level should be considered after assessing adherence to medication, knowledge of inhaler technique, and control of comorbid conditions and environmental factors. Stepping down may be appropriate for the child whose asthma has been well-controlled for several months and if no new or increased exposures to triggers are anticipated. For specifics regarding medications, see the Pharmacy & Medications System below. The following tables detail the medications recommended for each Step in each of the 3 age groups. (Click image to go to original document.)
Exercise-induced bronchospasm: In some children, exercise-induced bronchospasm (EIB) may be the only manifestation of asthma, and children with known asthma may experience worsening symptoms during physical exertion. EIB may begin during or after vigorous exercise and takes about 20 to 30 minutes to resolve after peak symptoms. EIB should be controlled so that it does not limit participation in sports. The severity of EIB will depend on the duration and vigor of exercise, dryness/coolness of the air, and factors intrinsic to the child.
Pre-treatment with inhaled beta2-agonists before exercise is successful in more than 80% of patients. In children with frequent symptoms, additional long-term control medications or stepping up treatment for children who have asthma in addition to EIB is indicated. Simple remedies, including warming-up before exercise and wearing a mask or scarf over the mouth when exercising in cold weather, may be helpful. Being physically fit helps postpone the onset of EIB in susceptible patients. Children with EIB alone should be monitored periodically by pulmonary function tests (PFTs) to ensure that they continue to have no evidence of asthma without exercise. [National: 2007] [Randolph: 2008]
Chronic cough: Chronic cough is a common presentation of asthma in children; if the cough is mainly nocturnal and has been present for greater than 2 weeks, response to a trial of asthma medication may raise suspicion of cough-variant asthma (CVA). [Johnson: 1991] This is particularly likely if there is a personal history of allergy and a family history of allergy and/or asthma. Medications may consist of bronchodilators, inhaled or oral corticosteroids, or leukotriene modifiers; no controlled studies to favor one class over the other have been performed. [Antoniu: 2007] [Todokoro: 2003]
Ongoing education: Education begins with in-office demonstrations for the patient and family on how to administer medication (see Administering Asthma Medication Video). The clinician also involves patients and their families in developing strategies for self-assessment, avoidance of triggers, and Asthma Action Plans for home and school. Ongoing education involves patient/family education (health literacy), school support, and referrals to local asthma resources, such as asthma camps or parent organizations. See Educational Goals for Asthma (EPR-3) (
 97 KB) for more
information on how to discuss asthma with patients and
families.
97 KB) for more
information on how to discuss asthma with patients and
families.Printable and online fillable Asthma Action Plans and other tools for educational purposes can be found under Asthma.
Specialty Collaborations & Other Services
A referral for specialty consultation and/or management should be considered if control has been erratic.
Pediatric Pulmonology (see NW providers [0])
Pediatric Allergy (see NW providers [1])
Departments of Health, State (see NW providers [0])
Pharmacy & Medications
 540 KB)
or 2020 Asthma Management Guidelines: Clinician's Guide (NHLBI) (
540 KB)
or 2020 Asthma Management Guidelines: Clinician's Guide (NHLBI) ( 2.1 MB).
Note that the GINA guidelines differ in not recommending use of SABAs alone,
rather recommending use also of inhaled ICS or instead use of ICS-LABA.
2.1 MB).
Note that the GINA guidelines differ in not recommending use of SABAs alone,
rather recommending use also of inhaled ICS or instead use of ICS-LABA.
 |
Comparative Dosages of Inhaled
Corticosteroids
from 2007 Asthma Care Quick Reference (EPR-3) (  719 KB) 719 KB)
|
 |
Usual Dosages of Other Long-Term Control
Medications
from 2007 Asthma Care Quick Reference (EPR-3) (  719 KB) 719 KB)
Click on images to download PDFs of the tables. |
Scheduled, daily inhaled corticosteroid (ICS) treatment is the preferred pharmacologic controller therapy forpersistent asthma in individuals of all ages. Intermittent ICS dosing includes treatment for brief periods, usually in response to symptoms or as an add-on with or without a long-acting beta2-agonist (LABA). Intermittent ICS use during upper respiratory tract infections are now recommended for patients 0-4 years of age with intermittent asthma. Decisions regarding which ICS to use should consider their differences in pharmacokinetic/pharmacodynamic properties, delivery, incidence of adverse effects, and cost to patient. Details on dosage and delivery are provided in 2020 Clinicians Guide - Intermittent Inhaled Corticosteroids (NHLBI) (
 356 KB).
356 KB).
Long-acting beta-2 agonists (LABA) should only be used in combination medications with inhaled corticosteroids. The 2020 Focused Updates recommend use of single maintenance and reliever therapy (SMART) for patients 4 years and older with a severe exacerbation in the past 12 months and who are not using ICS-salmeterol as maintenance therapy. SMART involves use of ICS-LABA (formoterol) in a single inhaler. Dosage varies by age, severity, and other factors. Detailed recommendations are provided in 2020 Clinicians Guide - SMART (NHLBI) (
 295 KB).
295 KB).Long-acting muscarinic antagonists (LAMA) are an acceptable alternative long-acting bronchodilator for a small subgroup of patients 12 years and older who cannot use a LABA due to intolerance, contraindication, inability to use device, or LABA is unavailable. Adding a LAMA to daily ICS therapy for those not controlled with ICS alone or ICS-LABA is recommended, though not in those with urinary retention or glaucoma. For detailed recommendations, see 2020 Clinician's Guide - LAMA (NHLBI) (
 218 KB).
218 KB). Leukotriene receptor antagonists (LTRA) may be considered as an alternative to ICS in mild persistent asthma or in step-up therapy along with ICS in patients who are not well-controlled with ICS alone. In mild persistent asthma, controlled trials have shown that ICS have greater efficacy and are more cost-effective than LTRA. However, montelukast has some advantages, including ease of administration, benefit in treating allergic rhinitis and exercise-induced bronchoconstriction, lack of demonstrated adverse effect on growth, and availability as a generic formulation. While a patient is more likely to have their best response to an ICS, some patients may respond equally well to a leukotriene receptor antagonist. Of note, neuropsychiatric events have been reported in adult, adolescent, and pediatric patients taking montelukast, and the clinical details of some post-marketing reports appear consistent with a drug-induced effect. The association with neuropsychiatric events has not been confirmed in subsequent studies, but should be monitored for when using this class of medication. LTRA were not considered in the 2020 NHLBI Report.
Immunology/Infectious Disease
Common allergens include dust mites, mold, cockroach feces, pollens, and exposure to animals. Dust mites, mold, and cockroach allergy are very rare in children and adults that grow up in the arid west because the humidity is generally too low to support those organisms. [Nelson: 1995] In children with seasonal allergies, asthma symptoms may worsen during certain pollen seasons. Symptoms can also flare as a result of mold exposure (e.g., during rainy seasons or in damp areas). While uncommon, food allergies can be a factor in asthma. Common food allergies in the US are eggs, cow's milk, wheat, soybean products, tree nuts, and peanuts. Food allergies that trigger symptoms of an asthma attack likely produce additional allergy symptoms (hives, rash, angioedema, nausea, vomiting, and/or diarrhea) followed by coughing and wheezing. Anaphylactic reactions require treatment with intramuscular epinephrine and monitoring in a medical setting.
Sensitization to allergens is determined by skin-prick testing or in-vitro measurement of allergen-specific IgE antibodies (sIgE). Third-generation sIgE assays, including ImmunoCAP, 3gAllergy, and Ultra-Sensitive EIA, have replaced radioallergosorbent testing (RAST) as the standard for quantitative sIgE testing. Allergen-specific IgE levels are not comparable across different testing modalities.
Management of allergens includes rational environmental avoidance strategies for at-risk populations. Though the evidence that allergen mitigation improves asthma outcomes is weak, such strategies may be beneficial, particularly for those with allergy to a specific indoor substance, such as dust mites. Multiple mitigation strategies are needed to improve outcome. When indicated by clinical history, allergen testing should be considered prior to embarking on mitigation strategies. The family’s ability to implement, and afford, the strategies should also be considered. For more detailed recommendations, see 2020 Clinician’s Guide - Indoor Allergen Mitigation (NHLBI) (
 140 KB).
140 KB).When allergen mitigation is not possible or ineffective, consider allergy immunotherapy. Antihistamines and nasal steroids, while helpful for allergies, are not effective for asthma. Studies suggest that immunotherapy may be appropriate when a causative allergen has been demonstrated. [Cox: 2011] Randomized controlled trials evaluating subcutaneous immunotherapy treatment (SCIT) in patients with asthma have demonstrated steroid-sparing effects and decreased bronchial hyperresponsiveness during the pollen season in appropriately selected patients. The 2020 Focused Updates recommend use of SCIT in patients 5 years and older with demonstrated allergic sensitization and worsening asthma symptoms following exposure to relevant antigen(s). SCIT should be administered in a clinical setting, ideally by an experienced pediatric allergist. Sublingual immunotherapy is not currently recommended. For more detailed recommendations, see 2020 Clinician’s Guide - Immunotherapy (NHLBI) (
 287 KB).
287 KB).Biologics may be useful as add-on therapy in patients with moderate to severe persistent allergic asthma who are inadequately controlled by optimal pharmacological therapy. Currently, omalizumab (anti-IgE) and mepolizumab (anti-IL-5) are approved for patients 6 years of age and older; benralizumab (anti-IL-5R) and dupilumab (anti-IL-4rα) are approved for patients 12 years of age or older. Biologic therapy should be initiated and monitored by a specialist with expertise in selecting patients most likely to respond to the agents and monitoring for side-effects.
Viral upper respiratory infections commonly trigger asthma exacerbations and may warrant a change in management of asthma symptoms. Limit infections through routine immunizations and teach preventive skills such as proper hand-washing. Some studies suggest that certain childhood viral infections, like rhinovirus, respiratory syncytial virus (RSV), and parainfluenza virus, can predispose children to developing asthma later in life. Consultation with an asthma specialist is recommended for patients with severe persistent asthma.
Specialty Collaborations & Other Services
Pediatric Allergy (see NW providers [1])
Complementary & Alternative Medicine
Ask the Specialist
Do you need lung function testing to diagnose asthma?
No, asthma can be diagnosed with clinical history. Lung function testing, such as spirometry with bronchodilator, or methacholine challenge testing, can confirm or rule out asthma.
Can younger patients use breath-actuated inhalers?
No, breath-actuated or dry-powder inhalers are not ideal for young patients due to lack of inspiratory pressure and suboptimal technique. Younger patients with asthma (ages 7 or less) should always be prescribed metered-dose inhalers with valved holding chambers for use.
Can infants be prescribed a metered-dose inhaler instead of nebulizer?
Yes, infants can be prescribed albuterol MDI. If the administration is correct, albuterol MDI has been shown to be as effective as nebulized albuterol.
What ICD-10 coding would you use for a child with viral-induced asthma severe enough to need controllers or hospitalizations?
ICD-10 provides codes specific for severity, as detailed in the NHLBI guidelines, and for exercise-induced, cough variant, and "other" asthma; the need for controllers and hospitalization would suggest at least moderate persistent asthma (J45.4) with a fifth digit to specify whether uncomplicated (0), with exacerbation (1), or with status asthmaticus (2). ICD10Data.com provides more detail (search for "asthma").
Resources for Clinicians
On the Web
2020 Asthma Management Guidelines: Clinician's Guide (NHLBI) ( 2.1 MB)
2.1 MB)
A 12-page summary of the 2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education
and Prevention Program Coordinating Committee Expert Panel Working Group; from the National Heart, Lung, and Blood Institute;
link will download as a pdf.
National Asthma Education and Prevention Program (NHLBI)
Offers links to information about asthma for providers, families, and schools; a program of the National Heart, Lung, and
Blood Institute.
Treating and Communicating About Asthma (NHLBI)
12-page summary of "Insights from Patients, Caregivers, and Health Care Providers" obtained through focus groups performed
in a 2020 qualitative research project; from the National Heart, Lung, and Blood Institute; downloadable as a pdf.
2021 Global Initiative for Asthma (GINA)
The GINA global strategy for asthma management and prevention is presented in its strategy documents, which are freely available
on the GINA Website.
Helpful Articles
Loughlin CE, Muston HN, Pena MA, Ren CL, Yilmaz O, Noah TL.
Pediatric Pulmonology year in review 2018: Asthma, physiology/pulmonary function testing, and respiratory infections.
Pediatr Pulmonol.
2019;54(10):1508-1515.
PubMed abstract
Patel SJ, Teach SJ.
Asthma.
Pediatr Rev.
2019;40(11):549-567.
PubMed abstract / Full Text
Davis CM, Apter AJ, Casillas A, Foggs MB, Louisias M, Morris EC, Nanda A, Nelson MR, Ogbogu PU, Walker-McGill CL, Wang J,
Perry TT.
Health Disparities in Allergic and Immunologic Conditions in Racial and Ethnic Underserved Populations: A Work Group Report
of the AAAAI Committee on the Underserved.
J Allergy Clin Immunol.
2021.
PubMed abstract
Ulrik CS, Lange P, Hilberg O.
Fractional exhaled nitric oxide as a determinant for the clinical course of asthma: a systematic review.
Eur Clin Respir J.
2021;8(1):1891725.
PubMed abstract / Full Text
Clinical Tools
Assessment Tools/Scales
Initial Asthma History Questions for Children (NHLBI) ( 57 KB)
57 KB)
Comprehensive list of questions for the initial assessment of a child with asthma; from the 2007 NHLBI Guidelines for Asthma
Diagnosis and Management.
Asthma Control Test for Children 4-11 Years Old (GlaxoSmithKline) ( )
)
A downloadable PDF version of the 7-question ACT to determine if a child’s asthma treatment plan is working.
Asthma Control Test for People 12 Years or Older (GlaxoSmithKline) ( 138 KB)
138 KB)
A self-administered, downloadable PDF version of the 5-question ACT to determine if the asthma treatment plan is working.
Asthma Control Test for Children & Adults (asthma.com)
Easy to use, online, asthma control test based on recent symptoms; allows for printing the results of the test; from asthma.com
(site sponsored by GlaxoSmithKline)
eAsthma Tracker
Tracking tool to help patients/families in self-assessing asthma symptoms to enable early recognition of worsening asthma
control; allows for notification of clinicians; developed by University of Utah/Intermountain Healthcare.
Propeller Sensors (propellerhealth.com)
Commercial product that uses sensors that attach to inhaler devices and a smart phone app to track medication use and environmental
factors and generates reports to help understand symptom patterns, control, and risk of exacerbations.
Care, Action, & Self-Care Plans
Asthma Action Plan (Intermountain Healthcare)
Sample of a 1-page plan in downloadable PDF.
Asthma Action Plans in Spanish, Chinese, Vietnamese, English (RAMP)
Asthma plans in printable and fillable PDF formats; Regional Asthma Management and Prevention program.
Care Processes & Protocols
Initial Visit - Classifying Asthma Severity and Initiating Treatment (NHLBI) ( 59 KB)
59 KB)
Table guides age-based classification of asthma severity and initiation of treatment, from the 2012 Asthma Care Quick Reference
summary of the 2007 NHLBI Guidelines.
Follow-Up Visits: Assessing Asthma Control & Adjusting Therapy (NHLBI) ( 56 KB)
56 KB)
A table of age-based classification of asthma control and steps in treatment; from the 2012 Asthma Care Quick Reference summary
of the 2007 NHLBI Guidelines.
Stepwise Approach for Managing Asthma Long Term (NHLBI) ( 4.6 MB)
4.6 MB)
A table of age-based medication treatment of asthma in 6 Steps; from the 2012 Asthma Care Quick Reference summary of the 2007
NHLBI Guidelines.
2020 Asthma Management Guidelines: At-a-Glance Guide (NHLBI) ( 540 KB)
540 KB)
A 6-page summary guide to treatment management based on the 2020 focused updates to the Asthma Management Guidelines: A Report
from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group; from the National
Heart, Lung, and Blood Institute.
2021 GINA Pocket Guide ( 3.0 MB)
3.0 MB)
Summary of the 2021 Global INitiative for Asthma guidelines for asthma management and prevention (for individuals 5 years
of age and older).
Medication Guides
Usual Dosages of Quick-Relief Medications for Asthma (NHLBI) ( 41 KB)
41 KB)
Details about the available choices of quick-relief (rescue) medications for asthma; from the Asthma Care Quick Reference
by the National Heart, Lung, and Blood Institute.
Comparative Dosages of Inhaled Corticosteroids (NHLBI) ( 63 KB)
63 KB)
Detailed comparisons; from the Asthma Care Quick Reference; National Heart, Lung, and Blood Institute.
Usual Dosages of Other Long-Term Control Agents (NHLBI) ( 51 KB)
51 KB)
Details on choices for long-term medications for asthma control other than inhaled corticosteroids, from the Asthma Care Quick
Reference by the National Heart, Lung, and Blood Institute.
Asthma Inhaler Poster (AAN/MoA)
A poster ($3 each) with pictures of available inhalers. Useful for learning and verifying with parents/patients the various
brands; Allergy & Asthma Network/Mothers of Asthmatics.
Questionnaires/Diaries/Data Tools
Patient Self-Assessment Record (NHLBI) ( 54 KB)
54 KB)
A sample record for patients to track asthma symptoms and medication use; from the 2007 National Heart, Lung, and Blood Institute
Guidelines.
Toolkits
Asthma Care Process Model (Intermountain Healthcare) ( )
)
Summarizes diagnosis and management information for asthma in pediatric and adult patients. Includes an algorithm, a model
for assessment of control, and a list of medications by age group and severity of symptoms; Intermountain Healthcare’s Primary
Care and Pediatric Specialty, 2016.
Other
Tools for Schools
Is the Asthma Action Plan Working? A Tool for School Nurse Assessment (NHLBI)
A brief checklist to determine how well an asthma action plan is working for a student. This tool can also be used by asthma
educators, primary care providers, and asthma specialists; National Heart, Lung, and Blood Institute.
Students with Chronic Illnesses: Guidance for Families, Schools, and Students (NHLBI)
Two-page guidance sheet presenting positive actions schools and families can take to address multiple chronic diseases. Facilitates
compliance with applicable Federal laws; National Heart, Lung, and Blood Institute.
How Asthma Friendly is Your Childcare Setting? (NAEPP)
Seven-item list that can be used by parents and child-care providers to help pinpoint specific areas that may cause problems
for children with asthma; National Asthma Education and Prevention Program.
Management of Asthma Exacerbations when a School Nurse is Not Available (NHLBI)
Offers a sample protocol for non-nursing staff, such as classroom teachers, who may need to help manage a child's asthma episode;
National Heart, Lung, and Blood Institute.
Management of Asthma Exacerbations – Emergency Nursing Protocol (NHLBI)
The 2-page document suggests emergency nursing protocol for students with
asthma symptoms who don’t have a personal asthma action plan; National Heart, Lung, and Blood Institute.
Spirometry360
Web-based program aimed at training office staff to perform optimal spirometry, provides feedback on technique and resulting
flow-volume loops via electronic connection, a program of the University of Washington Department of Pediatrics.
Patient Education & Instructions
Asthma Education Resources (EPA)
A number of educational resources for learning about asthma, managing triggers, and community action; Environmental Protection
Agency.
Peak Flow Meter Information (ALA)
Patient information regarding the use of peak flow meters for asthma control assessment; American Lung Association.
Breathing Easier with Asthma (Intermountain Healthcare) ( )
)
A 36-page pdf booklet to educate parents, families, and caregivers about asthma.
Breathing Easier With Asthma (Intermountain Healthcare) (Spanish) ( )
)
A comprehensive 36-page PDF about understanding and controlling asthma, in Spanish (Para Respirar Mas Facil Con Asma).
Peak Flow Meter Guide (Children's Minnesota)
Patient education on use of peak flow meters, includes expected results by height.
Resources for Patients & Families
FAQs and answers for parents can be found in For Parents and
Families at Asthma (FAQ).
How-to videos can be
found at:
- Using an Inhaler with a Spacer (Nationwide Children’s Hospital)
- Using a Dry Powder Inhaler (Nationwide Children’s Hospital)
- Using Spacers with a Mouthpiece (Nationwide Children’s Hospital)
- Using a Nebulizer (Nationwide Children’s Hospital)
- Using a Twisthaler (Nationwide Children’s Hospital)
- Using an EpiPen (Nationwide Children’s Hospital)
Information on the Web
Asthma in Children (MedlinePlus)
Information for families that includes description, frequency, causes, inheritance, other names, and additional resources;
from the National Library of Medicine.
Allergies & Asthma (healthychildren.org)
Focused on helping parents understand and live with pediatric asthma and allergies. Offers links to numerous online articles
and videos demonstrating use of inhalers and other devices; sponsored by the American Academy of Pediatrics.
Asthma (ALA)
Information for parents and families about asthma, asthma-friendly environments, advocacy, and more; American Lung Association.
Asthma (NHLBI)
Addresses multiple aspects of asthma, including causes, signs and symptoms, treatment, and prevention; National Heart, Lung,
and Blood Institute.
National & Local Support
Allergy & Asthma Network
A nonprofit that offers support for families affected by asthma.
Allergy & Asthma Network (Spanish)
A nonprofit that offers support in Spanish for families affected by asthma.
Studies/Registries
Clinical Trials in Children with Asthma (clinicaltrials.gov)
Studies looking at better understanding, diagnosing, and treating this condition; from the National Library of Medicine.
Asthma Research (ALA)
Current research projects funded by the American Lung Association. Emphasis on understanding the immune system’s role in asthma,
the effect of mold on severe asthma, improving treatment of severe asthma in children, and studying genes and their role
in controlling the immune response.
Services for Patients & Families Nationwide (NW)
| Service Categories | # of providers* in: | NW | Partner states (4) (show) | | NM | NV | RI | UT | |
|---|---|---|---|---|---|---|---|---|---|
| Camps for Children with Special Needs | 20 | 23 | 23 | 62 | 38 | ||||
| Departments of Health, State | 2 | 4 | 4 | 11 | |||||
| Local Support Groups, General | 2 | 9 | 38 | 8 | 63 | ||||
| National Support Services, General | 20 | 20 | 21 | 20 | 20 | ||||
| Pediatric Allergy | 1 | 8 | 8 | 12 | 6 | ||||
| Pediatric Pulmonology | 4 | 4 | 6 | 3 | |||||
| Pulmonary Function Testing | 3 | 1 | 5 | ||||||
For services not listed above, browse our Services categories or search our database.
* number of provider listings may vary by how states categorize services, whether providers are listed by organization or individual, how services are organized in the state, and other factors; Nationwide (NW) providers are generally limited to web-based services, provider locator services, and organizations that serve children from across the nation.
Authors & Reviewers
| Author: | Khanh Lai, MD, FAAP |
| Contributing Author: | Khalid Safi, MD |
| Reviewer: | Erik N. Newman, MD |
| 2020: update: Erik N. Newman, MDR |
| 2019: update: Khalid Safi, MDA; Khanh Lai, MD, FAAPA |
| 2013: update: Richard W. Hendershot, MDCA; Jennifer Goldman, MD, MRP, FAAPR; Derek A. Uchida, MDR; Chuck Norlin, MDA |
| 2008: update: Lynne M. Kerr, MD, PhDA; Deirdre Caplin, Ph.D., MSR; Derek A. Uchida, MDR |
| 2004: first version: Deirdre Caplin, Ph.D., MSA; Julia Rossi, RN, MSA |
Bibliography
Akinbami L.
The state of childhood asthma, United States, 1980-2005.
Adv Data.
2006(381):1-24.
PubMed abstract
U.S. Department of Health and Human Services Centers for Disease Control and Prevention Advance Data's statistics on asthma
in the United States from Vital and Health Statistics.
Antoniu SA, Mihaescu T, Donner CF.
Pharmacotherapy of cough-variant asthma.
Expert Opin Pharmacother.
2007;8(17):3021-8.
PubMed abstract
Asthma and Allergy Foundation of America.
Asthma Facts and Figures.
Asthma and Allergy Foundation of America; (2013)
http://www.aafa.org/display.cfm?id=8&sub=42.
The Asthma and Allergy Foundation of America (AAFA) is the leading patient organization for people with asthma and allergies,
and the oldest asthma and allergy patient group in the world.
Carrera-Bojorges XB, Pèrez-Romero LF, Trujillo-Garcìa JU, Jimènez-Sandoval JO, Machorro-Muòoz OS.
Internalization Disorders in Children with Asthma.
Rev Alerg Mex.
2013;60(2):63-68.
PubMed abstract
Cassimos DC, Tsalkidis A, Tripsianis GA, Stogiannidou A, Anthracopoulos M, Ktenidou-Kartali S, Aivazis V, Gardikis S, Chatzimichael
A.
Asthma, lung function and sensitization in school children with a history of bronchiolitis.
Pediatr Int.
2008;50(1):51-6.
PubMed abstract
Celeste Beck, MPH, Epidemiologist, Utah Asthma Program Kellie Baxter, BS, Health Program Specialist, Utah Asthma Program.
Asthma in Utah Burden Report.
Utah Department of Health, Utah Asthma Program.
2012.
The report assists in understanding the impact of asthma in Utah.
Chen W, Fitzgerald JM, Rousseau R, Lynd LD, Tan WC, Sadatsafavi M.
Complementary and alternative asthma treatments and their association with asthma control: a population-based study.
BMJ Open.
2013;3(9):e003360.
PubMed abstract / Full Text
Cloutier MM, Baptist AP, Blake KV, Brooks EG, Bryant-Stephens T, DiMango E, Dixon AE, Elward KS, Hartert T, Krishnan JA, Lemanske
RF Jr, Ouellette DR, Pace WD, Schatz M, Skolnik NS, Stout JW, Teach SJ, Umscheid CA, Walsh CG.
2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program
Coordinating Committee Expert Panel Working Group.
J Allergy Clin Immunol.
2020;146(6):1217-1270.
PubMed abstract / Full Text
The full 322-page report can be downloaded from the Full Text link above. Focused updates to the previous 2007 asthma management
guidelines on six priority topics. Note: The ages 0-4 stepwise approach table was updated in February 2021,
Cox L, Nelson H, Lockey R, Calabria C, Chacko T, Finegold I, Nelson M, Weber R, Bernstein DI, Blessing-Moore J, Khan DA, Lang
DM, Nicklas RA, Oppenheimer J, Portnoy JM, Randolph C, Schuller DE, Spector SL, Tilles S, Wallace D.
Allergen immunotherapy: a practice parameter third update.
J Allergy Clin Immunol.
2011;127(1 Suppl):S1-55.
PubMed abstract
Crapo RO, Casaburi R, Coates AL, Enright PL, Hankinson JL, Irvin CG, MacIntyre NR, McKay RT, Wanger JS, Anderson SD, Cockcroft
DW, Fish JE, Sterk PJ.
Guidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society
was adopted by the ATS Board of Directors, July 1999.
Am J Respir Crit Care Med.
2000;161(1):309-29.
PubMed abstract / Full Text
Davis CM, Apter AJ, Casillas A, Foggs MB, Louisias M, Morris EC, Nanda A, Nelson MR, Ogbogu PU, Walker-McGill CL, Wang J,
Perry TT.
Health Disparities in Allergic and Immunologic Conditions in Racial and Ethnic Underserved Populations: A Work Group Report
of the AAAAI Committee on the Underserved.
J Allergy Clin Immunol.
2021.
PubMed abstract
Elazab N, Mendy A, Gasana J, Vieira ER, Quizon A, Forno E.
Probiotic Administration in Early Life, Atopy, and Asthma: A Meta-analysis of Clinical Trials.
Pediatrics.
2013;132(3):e666-76.
PubMed abstract
Conclusion: Prenatal and/or early-life probiotic administration reduces the risk of atopic sensitization and decreases the
total IgE level in children but may not reduce the risk of asthma/wheeze. Follow-up duration and strain significantly modified
these effects. Future trials for asthma prevention should carefully select probiotic strain and consider longer follow-up.
Galil N.
Depression and asthma in children.
Curr Opin Pediatr.
2000;12(4):331-5.
PubMed abstract
Gillette C, Loughlin CE, Sleath BL, Williams DM, Davis SD.
Quality of pulmonary function testing in 3 large primary care pediatric clinics in rural North Carolina.
N C Med J.
2011;72(2):105-10.
PubMed abstract
Johnson D, Osborn LM.
Cough variant asthma: a review of the clinical literature.
J Asthma.
1991;28(2):85-90.
PubMed abstract
Kercsmar C.M., Mcdowel K.M.
Kendig's Disorders of the Respiratory Tract in Children. Chapter 45: 45 - Wheezing in Older Children: Asthma.
Ninth Edition ed. Elsevier;
2019.
978-0323448871
Leyenaar JK, Ralston SL, Shieh MS, Pekow PS, Mangione-Smith R, Lindenauer PK.
Epidemiology of pediatric hospitalizations at general hospitals and freestanding children's hospitals in the United States.
J Hosp Med.
2016;11(11):743-749.
PubMed abstract / Full Text
Loughlin CE, Muston HN, Pena MA, Ren CL, Yilmaz O, Noah TL.
Pediatric Pulmonology year in review 2018: Asthma, physiology/pulmonary function testing, and respiratory infections.
Pediatr Pulmonol.
2019;54(10):1508-1515.
PubMed abstract
National Asthma Education and Prevention Program Expert Panel.
Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma - Summary Report 2007.
National Institutes of Health: National Heart, Lung, and Blood Institute; (2007)
https://www.nhlbi.nih.gov/sites/default/files/media/docs/asthsumm.pdf. Accessed on 03/24/2021.
A 60-page summary of the 440-page comprehensive guideline; published by the National Heart, Lung, and Blood Institute.
National Asthma Education and Prevention Program Expert Panel.
Expert Panel Report 3 (EPR3): Guidelines for the Diagnosis and Management of Asthma.
National Heart Lung and Blood Institute, NIH; (2007)
https://www.nhlbi.nih.gov/health-topics/guidelines-for-diagnosis-manag.... Accessed on 6/24/2021.
For the full 440-page report, click the Download PDF 4 MB button; from the National Heart Lung and Blood Institute, National
Institutes of Health. A 60-page Summary Report and a 12-page Asthma Care Quick Reference are also downloadable from the same
web page.
Nelson HS, Fernandez-Caldas E.
Prevalence of house dust mites in the Rocky Mountain states.
Ann Allergy Asthma Immunol.
1995;75(4):337-9.
PubMed abstract
Oxford Journals - Oxford University Press.
Obesity and the Risk of Newly Diagnosed Asthma in School-age Children.
Journal of Epidemiology.
2013;vol. 158.
/ Full Text
Adjusted relative risk of new-onset asthma by percentile of body mass index and weight status, Children’s Health Study, 1993–1998*
Paris J, Peterson EL, Wells K, Pladevall M, Burchard EG, Choudhry S, Lanfear DE, Williams LK.
Relationship between recent short-acting beta-agonist use and subsequent asthma exacerbations.
Ann Allergy Asthma Immunol.
2008;101(5):482-7.
PubMed abstract / Full Text
Patel SJ, Teach SJ.
Asthma.
Pediatr Rev.
2019;40(11):549-567.
PubMed abstract / Full Text
Perry R, Braileanu G, Palmer T, Stevens P.
The Economic Burden of Pediatric Asthma in the United States: Literature Review of Current Evidence.
Pharmacoeconomics.
2019;37(2):155-167.
PubMed abstract / Full Text
Philp JC, Maselli J, Pachter LM, Cabana MD.
Complementary and alternative medicine use and adherence with pediatric asthma treatment.
Pediatrics.
2012;129(5):e1148-54.
PubMed abstract / Full Text
Prasad B, Nyenhuis SM, Weaver TE.
Obstructive sleep apnea and asthma: Associations and treatment implications.
Sleep Med Rev.
2013.
PubMed abstract
Randolph C.
Exercise-induced Bronchospasm In Children.
Clin Rev Allergy Immunol.
2008;34(2):205-16.
PubMed abstract
Reddel HK et al.
2021 GINA Report, Global Strategy for Asthma Management and Prevention.
Global Initiative for Asthma.
2021.
/ https://ginasthma.org/gina-reports/
A downloadable 217-page report with guidelines for the care of children (and adults) with asthma from the World Health Organization.
A "What's New in 2021" report. GINA does not distinguish between mild persistent asthma and intermittent asthma.
Samuel J. Arbes, Jr., DDS, MPH, PhD, Peter J. Gergen, MD, MPH, Ben Vaughn, MS,3 and Darryl C. Zeldin, MD.
US National Library of Medicine National Institutes of Health: Asthma Cases Attributable to Atopy: Results from the Third
National Health and Nutrition Examination Survey.
PMC.
2008.
/ Full Text
Conclusion: About half of the current asthma cases in the U.S. population represented by NHANES III were attributable to atopy.
Some allergen-specific skin tests were not independently associated with asthma.
Sears MR, Johnston NW.
Understanding the September asthma epidemic.
J Allergy Clin Immunol.
2007;120(3):526-9.
PubMed abstract
Todokoro M, Mochizuki H, Tokuyama K, Morikawa A.
Childhood cough variant asthma and its relationship to classic asthma.
Ann Allergy Asthma Immunol.
2003;90(6):652-9.
PubMed abstract
Ulrik CS, Lange P, Hilberg O.
Fractional exhaled nitric oxide as a determinant for the clinical course of asthma: a systematic review.
Eur Clin Respir J.
2021;8(1):1891725.
PubMed abstract / Full Text
University of Virginia Health System.
Children With Asthma Often Suffer Developmental And Behavioral Problems.
Science Daily; (2013)
http://www.sciencedaily.com/releases/2007/04/070412163840.htm. Data for the research came from the National Survey of Children's Health 2003, which was obtained from the Centers for Disease
Control and Prevention (CDC) National Center for Health Statistics.. Accessed on 3/24/2021.
Data for the research came from the National Survey of Children's Health 2003, which was obtained from the Centers for Disease
Control and Prevention (CDC) National Center for Health Statistics.
Weinberger M.
Time for a New Paradigm for Asthma Management.
Mayo Clin Proc.
2016;91(4):405-7.
PubMed abstract
Yang IV, Lozupone CA, Schwartz DA.
The environment, epigenome, and asthma.
J Allergy Clin Immunol.
2017;140(1):14-23.
PubMed abstract / Full Text